Your Heart Isn’t Trying to Surprise You: Learning the Language of Your Body’s Warnings

Your heart has been sending you messages for weeks, maybe months—but you’ve been hitting ‘ignore.’ It’s easy to do. That weird twinge in your chest? You think it’s just stress. The sudden shortness of breath? Must be that you’re getting older. Because of this, many people miss the heart warning signs their body is giving them.
It’s natural to fear overreacting, but that fear keeps you from getting help. You feel confused about which symptoms actually matter and which ones are harmless. But here’s the truth: most heart attacks have warning signs that appear days or weeks before the emergency. Your heart tries to tell you something is wrong.

In this guide, you will learn the difference between serious heart warning signs and minor aches. We’ll show you the specific signals that point to heart problems. You’ll know how to tell when to simply call your doctor versus when to call 911 right away.
Knowing these early detection techniques is a powerful tool for protecting your cardiovascular health. You’ll understand why your heart “warns” before most emergencies and how to use simple methods to monitor your health.
Why Your Heart Sends Warning Signals Before Emergencies
Your heart is like a car’s check engine light. It warns you before it breaks down.
Here’s what happens inside your body. When plaque builds up in your arteries, less blood flows to your heart. Less blood means less oxygen. Your body feels this drop in oxygen and sends you symptoms. That chest pressure? That’s your heart saying “I need help.”

Most people think heart attacks come out of nowhere. They don’t. Plaque takes 20 to 30 years to build up in your arteries. The “sudden” heart attack? It’s actually the final event after decades of slow damage.
The numbers tell an important story. Half of all heart attack victims felt warning signs in the month before it happened. Two out of three women noticed unusual tiredness weeks earlier. But most people ignored these signs for an average of 5 hours before getting help.

Those 5 hours matter more than you think. Doctors can prevent 80% of heart attacks if you catch the early warning signs of heart disease. Your heart doesn’t ambush you. It tells you something’s wrong.
There are two types of warnings you need to know. Chronic warnings build slowly over weeks—like getting tired easier or feeling short of breath climbing stairs. Acute warnings hit fast and hard—like sudden chest pain or cold sweats. Both are cardiovascular warning signals worth paying attention to.
The Silent Warning Signs Most People Miss
The most dangerous heart warning signs are the ones that seem normal.
Unusual Tiredness That Won’t Go Away
Sarah, 52, blamed her exhaustion on work stress for three weeks. She felt wiped out after simple tasks like making dinner or folding laundry.

This wasn’t normal tired—it was her heart struggling to pump enough oxygen-rich blood to her muscles. When your heart can’t deliver oxygen efficiently, your whole body feels drained.
Test yourself: If you’re more tired than usual for no clear reason, and rest doesn’t help, pay attention.
Getting Winded During Normal Activities
You’ve climbed these stairs a hundred times. But today you’re breathing hard halfway up. When arteries narrow, your heart works harder to pump blood, and you feel it as breathlessness.

This is one of the most common early warning signs of heart disease.Women are 50% more likely than men to experience this instead of chest pain.
Waking Up Gasping for Air
You bolt awake feeling like you can’t breathe. Or you need three pillows to sleep comfortably. Your heart may be struggling to pump blood when you lie flat, causing fluid to back up into your lungs.
Pain in Weird Places
Your jaw aches. Your shoulder throbs. Your neck feels stiff. No injury explains it. Heart problems often show up as pain that radiates from your chest to your jaw, neck, shoulders, or back.

Your brain can misinterpret where the pain is coming from.This happens because your heart shares nerve pathways with these areas.
“Indigestion” That Feels Off
You think it’s heartburn. You pop antacids. But this burning in your chest or upper belly won’t quit.

Many people mistake heart attack symptoms for stomach problems because the sensations feel similar.
If antacids don’t help and the feeling persists, don’t assume it’s just indigestion.
Sudden Anxiety or Dread
You feel panic for no reason. Your heart races. You’re sweating. This isn’t just anxiety—your body releases stress hormones when your heart isn’t getting enough oxygen.

It’s a physiological response, not just in your head.Many people go to the ER thinking they’re having a panic attack when it’s actually their heart.
Cold Sweats Out of Nowhere
You’re suddenly drenched in sweat, but you’re not hot or exercising. Cold sweats appear in 30% of women having heart attacks. Your nervous system goes into overdrive when your heart is in trouble.

Women: If you experience any three of these symptoms together, call your doctor today. Don’t wait to see if they go away. These are your heart’s early warnings before something worse happens.
The key to recognize heart attack symptoms? They feel different from anything you’ve experienced before. Trust that feeling.
Warning Signs Checklist:
- Fatigue that doesn’t match your activity level
- Breathlessness climbing stairs or walking
- Waking up short of breath
- Unexplained jaw, neck, or shoulder pain
- “Indigestion” that won’t respond to antacids
- Sudden anxiety with physical symptoms
- Cold sweats without obvious cause
Remember: These symptoms seem innocent. That’s exactly why they’re dangerous.
Risk Factors That Make Warning Signs More Serious
Some people need to pay closer attention to heart warning signs than others. Here’s why.
Count Your Risk Factors
Grab a pen. Check off everything that applies to you. This matters more than you think.

You Can’t Change These:
- Your parent or sibling had heart disease before age 55
- You’re a man over 45 or a woman over 55
- You have a family history of early heart attacks
If your dad had a heart attack at 50, your risk jumps 50% to 100%. That’s not a small increase. When you have family history, even minor symptoms deserve a doctor’s visit.
You Can Change These:
- High blood pressure (over 130/80)
- High cholesterol
- Diabetes or prediabetes
- Current smoker or quit within 10 years
- Overweight (BMI over 25)
- You sit most of the day
Diabetes doubles your heart disease risk. Smoking causes 20% of all heart disease deaths. High blood pressure damages your arteries every single day, even when you feel fine.
Why Multiple Risk Factors Change Everything

Here’s what most people get wrong. Risk factors don’t add up—they multiply. If you have three or more risk factors, your risk isn’t three times higher. It’s ten times higher.
Think of it like this. One risk factor is a crack in your foundation. Three risk factors? Your whole house is unstable. Those early warning signs of heart disease become urgent warnings when you’re already at high risk.
Let’s say you feel unusually tired for a week. If you’re 35 with no risk factors, your doctor might watch and wait. But if you’re 55 with diabetes and high blood pressure? That’s a same-day appointment.
What This Means for You
More risk factors = lower bar for seeking medical care. You don’t get to wait and see if symptoms go away. When you have multiple risk factors, those cardiovascular warning signals are louder and more urgent.

Your action plan depends on your count:
- 0-1 risk factors: Pay attention to symptoms lasting more than a week
- 2-3 risk factors: See your doctor for new symptoms within 2-3 days
- 4+ risk factors: Any new symptom deserves immediate medical evaluation
The good news? Five of those risk factors can be changed. You’re not stuck with your current risk level. Every improvement you make lowers the threshold of danger.
But right now, today, know your number. Count your risk factors. That number tells you how seriously to take every symptom your body sends.
Quick Self-Assessment:
How many of these apply to you? □ Family history of early heart disease □ Age (men >45, women >55) □ High blood pressure □ High cholesterol □ Diabetes or prediabetes □ Current or recent smoker □ Overweight or obese □ Sedentary lifestyle
Your score:
- 0-1: Stay aware of symptoms
- 2-3: Be proactive with new symptoms
- 4+: Treat every new symptom as urgent
Remember: More risk factors mean warning signs matter more, not less
When to Call Your Doctor vs. When to Call 911
The fear of overreacting stops more people than overreacting ever would. Here’s your clear decision guide.
Call 911 Right Now If You Have:
Chest pain or pressure lasting more than 5 minutes. Don’t wait to see if it goes away. Don’t drive yourself to the hospital. Every hour you delay treatment, your chance of dying goes up 7%. Doctors call it “time is muscle” because your heart tissue dies without blood flow.
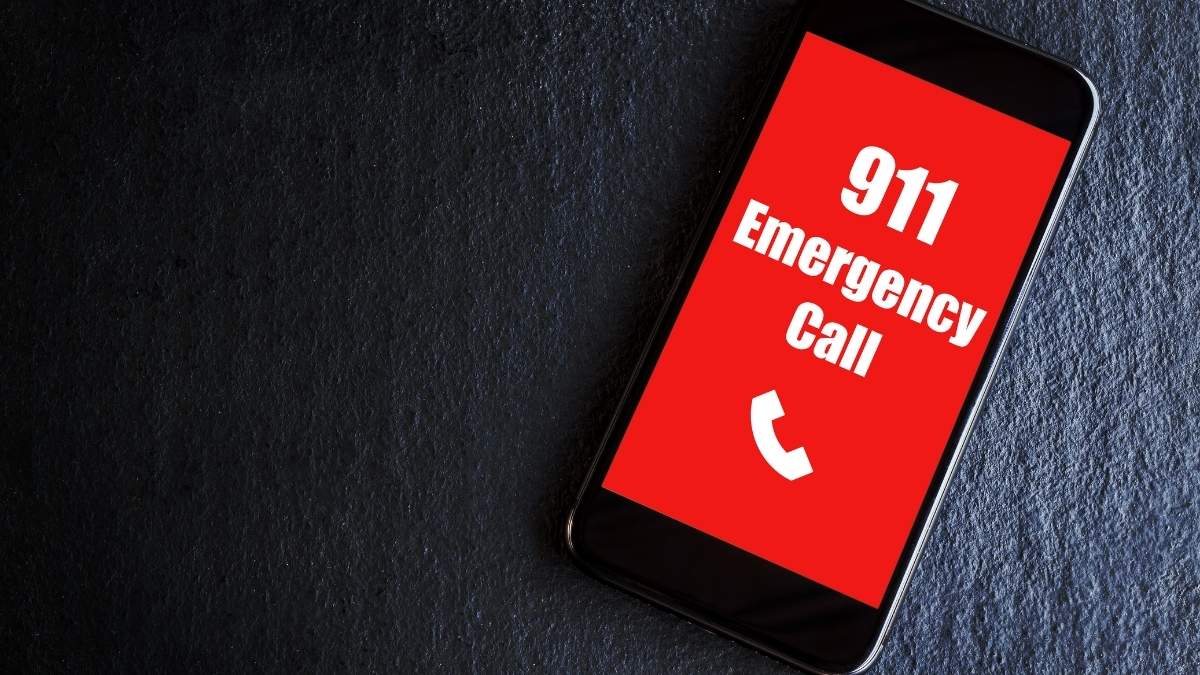
Sudden severe symptoms like crushing chest pain, can’t catch your breath, or feel like you’re dying. When heart attack symptoms hit hard and fast, minutes matter more than anything else.
Loss of consciousness, even for a few seconds. This means your brain isn’t getting enough blood. Call 911 immediately.
Pain spreading to your jaw, neck, arms, or back along with chest discomfort, sweating, or nausea. These are classic signs to recognize heart attack symptoms in action.
What Actually Happens When You Call 911
You tell the operator “chest pain.” They ask a few quick questions. An ambulance arrives in minutes. Paramedics run an EKG right there in your living room. They call ahead to the hospital so the cardiac team is ready when you arrive.
Here’s what most people don’t know: Paramedics can start life-saving treatment before you reach the hospital. You get help 30-60 minutes faster than if someone drives you.
Yes, 30% of chest pain calls turn out to be false alarms. That’s expected. That’s acceptable. Emergency doctors would rather see ten false alarms than miss one real heart attack.
Call Your Doctor Today (Same-Day Appointment) If:
First-time chest discomfort that comes and goes. Even if it’s mild. Even if it only lasted a minute. New heart warning signs need evaluation within 24 hours.

Palpitations lasting more than 30 minutes. Your heart racing or skipping beats occasionally is normal. Racing for half an hour isn’t.
Sudden increase in symptoms you’ve had before. Your usual shortness of breath got worse. Your fatigue went from manageable to can’t-get-out-of-bed. Changes in patterns matter.
Schedule an Appointment This Week If:
Unusual tiredness that’s lasted more than a few days. Not “I stayed up late” tired. More like “something feels wrong” tired.

You’re getting winded easier than before. Stairs that never bothered you now leave you breathless.
Intermittent symptoms that keep coming back. Occasional chest tightness. On-and-off jaw pain. Your body is trying to tell you something.
The Embarrassment Factor
“What if it’s nothing?” So what? You’re alive to feel embarrassed. That’s a win.
“I don’t want to waste their time.” You’re not. This is literally what 911 operators and paramedics do all day. They’re trained specifically for chest pain calls.

“It’s probably just anxiety.” Maybe. But many people sitting in ERs right now thought the same thing. They were having heart attacks.
The hard truth: People die from embarrassment. They wait because they don’t want to seem dramatic. They convince themselves it’s probably nothing. Then it’s too late.
Money Shouldn’t Stop You
An ambulance costs money. A funeral costs more. Most insurance covers emergency cardiac care.

Even without insurance, hospitals have payment plans and financial assistance.More importantly: If you’re having a heart attack, you need to be alive to worry about the bill. Deal with costs later. Stay alive first.
Your Quick Decision Tree

Severe, sudden, or lasting >5 minutes? → Call 911
New symptom or first-time discomfort? → Call doctor today
Getting worse or changing pattern? → Call doctor today
Mild and intermittent but concerning? → Appointment this week
When in doubt? → Call your doctor and describe what you feel. Let them decide if you need to come in or call 911.
Remember: False alarms save more lives than missed calls ever will.
Emergency Symptoms (Call 911):
- Chest pain/pressure >5 minutes
- Sudden severe shortness of breath
- Fainting or near-fainting
- Pain spreading to jaw, neck, or arms
- Cold sweats with chest discomfort
Urgent Symptoms (Doctor Today):
- First-time chest discomfort
- Heart racing >30 minutes
- Sudden worsening of known symptoms
Important Symptoms (Doctor This Week):
- New unexplained fatigue
- Increasing breathlessness
- Intermittent chest discomfort
The Rule: If you’re reading this trying to decide, pick up the phone. That hesitation? That’s your answer.
What Keeps You Up at Night?
Many people worry about their cardiovascular health but don’t know if a sudden chest ache is just stress or an early warning sign of heart disease. If your body is screaming at you all the time, it’s hard to hear the important heart warning signs.
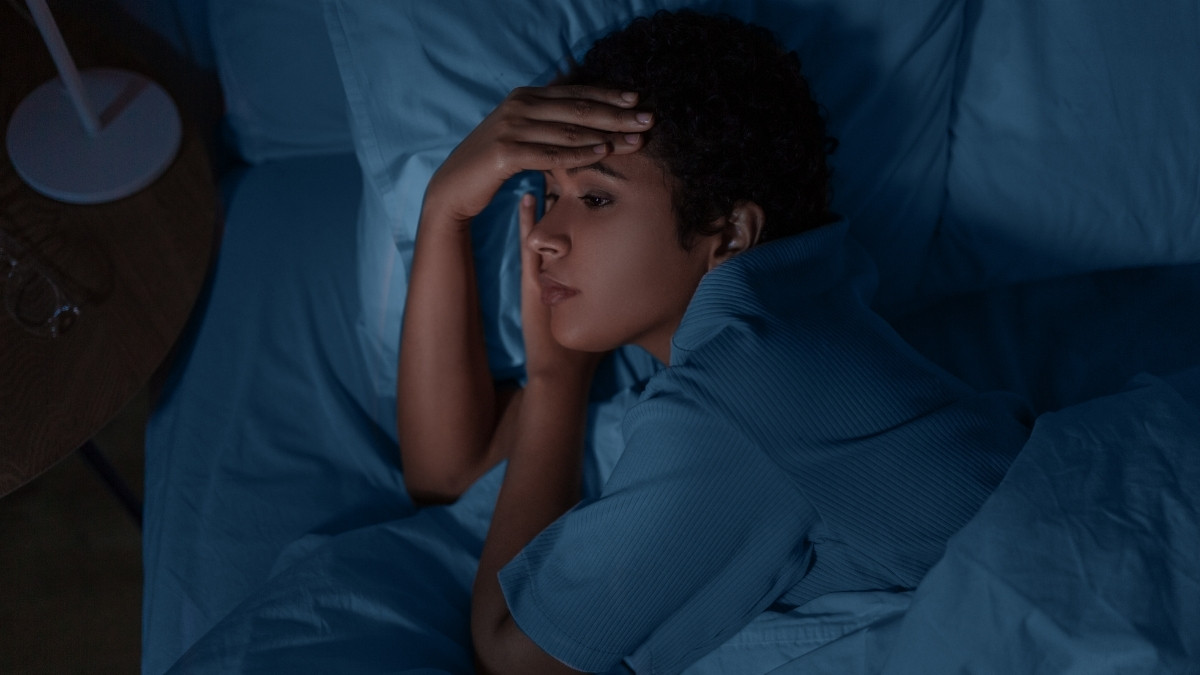
Think of your body like a radio: if there’s too much static, you can’t hear the song clearly. Lifestyle changes help you “tune in” to your body’s signals, reducing the noise so you can hear the important messages.
Tuning Into Your Heart’s Signals
Making simple changes helps you hear your body better and spot problems sooner. This lessens the chance that you will miss key heart warning signs. It’s about consistency, not being perfect every day.
Daily Activity Clears the Feedback
When you exercise regularly, your heart and blood vessels get stronger. A fitter body is better at sending and receiving information.

You become more aware of how your heart feels during activity. This means you will notice problems sooner, like getting winded much faster than usual.
Just 30 minutes of walking daily reduces your heart disease risk by 30 to 40%.
Calm Your Mind to Hear Your Heart
Stress management is key because stress can copy heart warning signs. Things like anxiety can cause a racing heart or chest tightness, which makes for a lot of symptom confusion.

When you manage your stress, you reduce this background noise. This helps you tell the difference between feeling stressed and a true physical problem.
Good Sleep Clears the Line
Quality sleep allows your body to signal properly. When you are tired, your system is running on low power and can’t communicate well.

If you have a condition like sleep apnea, which increases your heart attack risk two to three times, getting it treated significantly improves your overall cardiovascular health.
Weight and Vices Matter
Carrying extra weight raises your symptom baseline. This means your body is already working harder, and you might miss a new, abnormal sign because your usual state already felt strained.

Losing even 10% of your body weight significantly improves cardiovascular health. Also, limiting alcohol and quitting smoking takes major burdens off your heart, reducing the “static” and making your body’s true signals clearer.
These consistent, helpful choices work together to help you quickly recognize abnormal signs. When your heart is healthy, the signals are clear. Less noise means clearer early warning signs of heart disease.
Final Thought:
Your Heart Has Been Speaking to You All Along
We’ve learned that your heart gives early warning signs before most major events. Tiny, subtle symptoms matter, especially things like new fatigue, breathlessness, or digestive issues. Writing these things down helps you see patterns. Your personal risk factors lower the threshold for when you should seek care. If you are ever in doubt, call your doctor. For severe, sudden symptoms, call 911 immediately.
Recognizing heart warning signs isn’t about paranoia—it’s about partnership with your body.
Start today: Track your normal resting heart rate and blood pressure. Notice how you feel during your normal daily activities. If something changes and doesn’t go away, don’t dismiss it. This is an ongoing journey for your cardiovascular health. Your heart has been speaking to you all along—now you know how to listen. Share this article with someone who needs to hear their heart’s message.
Don’t miss the signs! Learn the heart warning signs your body sends days or weeks before an emergency. Improve your cardiovascular health with early detection.