Scientists Uncover the Surprising Age When Your Heart Health Declines Fastest (Check Your Age Now)

If you think heart disease is something to worry about in your 60s or 70s, groundbreaking research from University College London reveals you might be missing the most critical window by decades.
Most people treat their 30s and 40s like safe years for their heart. They figure heart problems come later, so why stress about cardiovascular health now? But scientists tracked nearly 6,000 people for 25 years and found something alarming.
The damage that happens during middle age—specifically between 45 and 69—sets up a trajectory that predicts not just heart attacks, but dementia decades later.
This is when heart health decline age matters most. Miss this window, and you’re fighting an uphill battle for the rest of your life.
Here’s what you’ll learn: the exact age range when your heart ages fastest, why middle age heart health predicts your brain function at 80, the blood test that shows silent heart damage 25 years before symptoms appear, and eight actions backed by science that you can start today.
Your heart and brain are more connected than you think. What you do right now determines both.
Scientists Uncover the Surprising Age When Your Heart Health Declines Fastest
The Critical Age Window: Why 45-69 Matters More Than You Think
Your heart doesn’t age the same way every decade. Scientists at University College London discovered something shocking: the years between 45 and 69 are when your heart health drops fastest. This matters way more than you think.

The research team tracked nearly 6,000 people for 25 years—starting in 1985. They measured a protein called troponin that shows up when your heart muscle gets damaged.
People in their 40s, 50s, and 60s with high troponin levels had a 38% higher chance of getting dementia later in life. By age 80, their brains worked like they were 1.5 years older. By 90, they’d lost 2 years of mental sharpness.
Here’s the scary part: this damage happens silently. You feel fine. No chest pain. No warning signs. But 15 years later, brain scans show a smaller hippocampus—that’s your memory center.
Of the 695 people who developed dementia in the study, researchers say 17% could have prevented it by protecting their heart health in middle age.
Think about it this way: A healthy 50-year-old and a 50-year-old with high troponin look the same today. But at 80? One remembers their grandkids’ names easily. The other struggles.
Your cardiovascular health in your 40s and 50s sets up everything that follows. Miss this window, and you’re playing catch-up for decades.
But what exactly is changing in your heart during these years? The answer lies in a protein most people have never heard of.
The Hidden Biomarker Predicting Your Heart’s Future
Troponin is a protein your heart releases when its muscle cells get damaged. Think of it like a smoke detector instead of a fire alarm. A fire alarm screams during a heart attack. A smoke detector catches tiny problems early.
New high-sensitivity tests spot troponin levels way below heart attack range. This catches subclinical heart damage—silent damage you can’t feel. No chest pain. No symptoms. Just slow wear and tear.
Here’s why this matters for your brain: your heart and brain share the same blood vessel network. When your heart struggles, less blood reaches your brain. After 15 years, people with high troponin showed smaller hippocampus size on MRI scans. That’s your memory control center shrinking.
The Hidden Biomarker
Long-Term Result: Smaller hippocampus size (memory center shrinking). Damage one, damage all.
Your blood vessels feed every organ. Damage one system, you damage them all.
Now that you understand what’s happening inside your body, let’s look at what factors speed up this decline—and which ones you can control.
Your Heart Age vs. Your Real Age: Understanding the Gap
You might be 45 on your birthday, but your heart could be 55. The American Heart Association created a heart age calculator that shows how old your cardiovascular system really is based on your risk factors. And for most people, the news isn’t great.
Researchers tested over 14,000 adults between ages 30 and 79 using this tool. None of them had been diagnosed with heart disease yet. The results were eye-opening. Women’s hearts averaged 55.4 years old, but their actual age was only 51.3—a 4-year gap. Men had it worse. Their hearts averaged 56.7 years old while they were only 49.7—a 7-year difference.
The gaps got bigger when researchers looked at different groups. Black men’s hearts aged 8.5 years faster than their bodies. Hispanic men showed a 7.9-year gap. White men had a 6.4-year difference. For women, Black women’s hearts were 6.2 years older, Hispanic women 4.8 years older, and White women 3.7 years older than their actual age.
This happens because of lifestyle and risk factors that pile up over time. High blood pressure. Extra weight. Poor diet. Smoking. Lack of exercise. Each one ages your heart faster than the calendar does.
Age-O-Meter
The American Heart Association now uses something called the PREVENT calculator for cardiovascular health assessment. It looks at your cholesterol, blood pressure, blood sugar, smoking status, and other heart disease risk factors. Then it tells you your heart’s real age and your risk of having a heart attack or stroke in the next 10 years.
Why does this number matter? Because seeing “your heart is 10 years older” hits different than hearing “your cholesterol is a bit high.” It makes the risk real. Personal. Urgent.
These numbers might seem alarming, but here’s the encouraging part: nearly all factors affecting your heart age are within your control.
Life’s Essential 8: The Science-Backed Framework for Heart Health
The American Heart Association studied what actually keeps hearts healthy. They identified eight specific factors that determine how long you’ll live and how well your heart works.
They call it Life’s Essential 8, and the research behind it is solid. For every 10-point improvement in your total score, your risk of heart disease drops by 22-40%.
Each factor gets scored from 0 to 100 points. Higher is better. Here’s what matters most:
1. Diet Quality

Eat like people in Mediterranean countries do. Lots of fruits, vegetables, whole grains, and fish. Use olive or canola oil instead of butter. Add nuts and seeds. Cut back on red meat and processed foods. This isn’t about being perfect—it’s about making better choices most of the time.
2. Physical Activity

Move for 150 minutes per week at moderate intensity, or 75 minutes if you’re doing vigorous exercise. That’s just 30 minutes, five days a week. Mix cardio with strength training. Even short walks count. Your body needs daily movement to keep your cardiovascular health metrics in the healthy range.
3. Nicotine Exposure

This is the leading cause of preventable death. Period. That includes cigarettes, e-cigarettes, vaping, and secondhand smoke. If you smoke, quitting is the single best thing you can do for your heart. No exceptions.
4. Sleep Health

This is new to the list, added because research proved sleep matters as much as diet and exercise. Get 7-9 hours every night. Poor sleep raises your blood pressure, increases inflammation, and makes other health problems worse. Good sleep hygiene means consistent bedtimes, dark rooms, and cool temperatures.
5. Body Mass Index
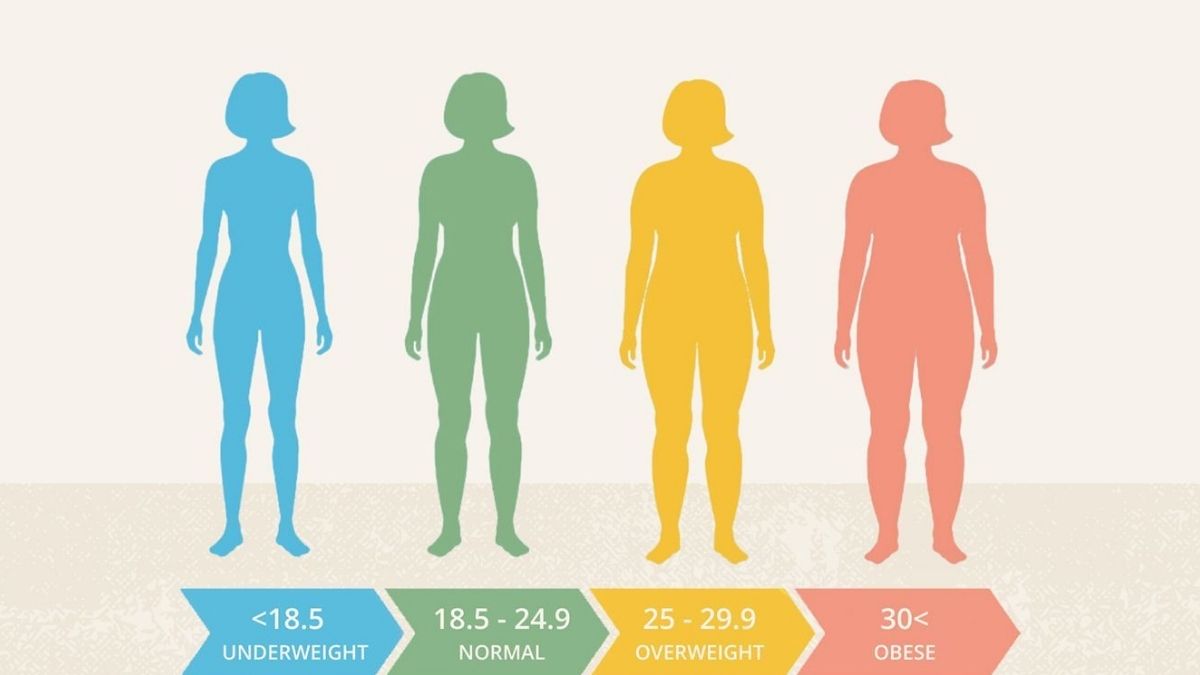
Keep your BMI under 25 if possible. Extra weight makes your heart work harder and increases your risk for diabetes, high blood pressure, and high cholesterol. Small weight loss—even 5-10 pounds—makes a real difference.
6. Blood Lipids
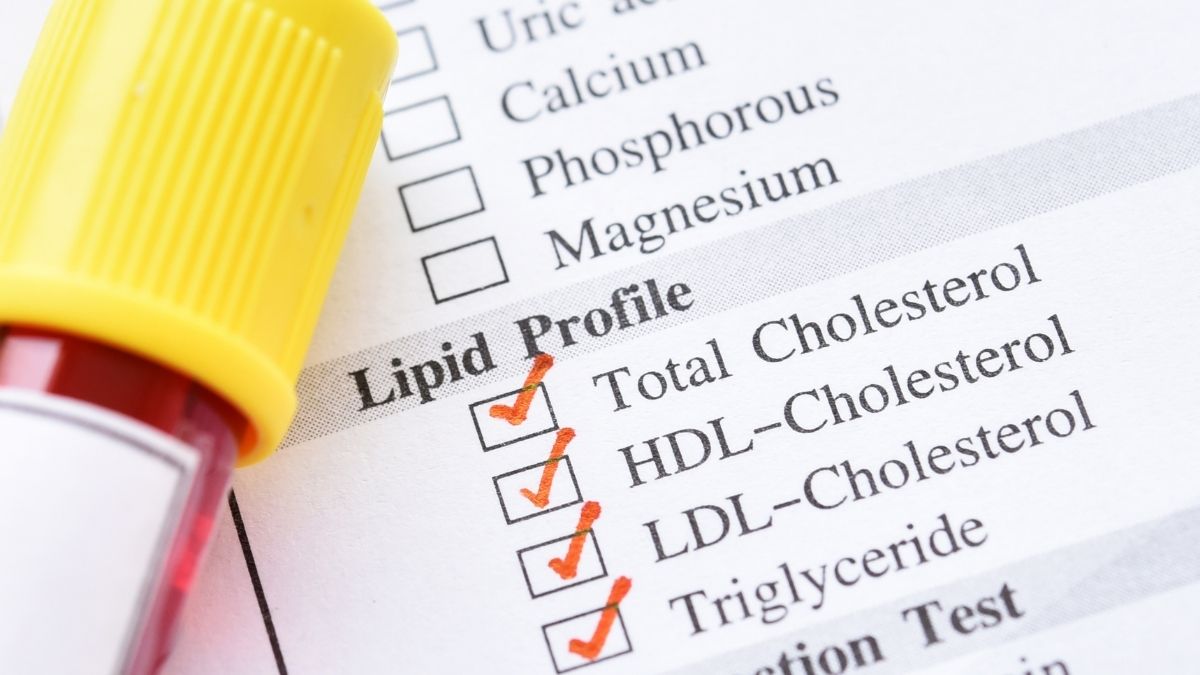
Your non-HDL cholesterol should stay under 130 mg/dL. This number shows how much bad cholesterol is building up in your arteries. Diet helps, but some people need medication. That’s okay. Taking a statin is better than having a heart attack.
7. Blood Glucose

High blood sugar damages your blood vessels over time. Your HbA1c test shows your average blood sugar over three months. Keeping it in a healthy range prevents diabetes and protects your heart.
8. Blood Pressure

Aim for under 120/80. High blood pressure is the number one risk factor for stroke. It quietly damages your arteries for years before you notice any symptoms. Check it regularly. If it’s high, work with your doctor on heart disease prevention strategies.
Understanding these metrics is one thing—but implementing them in your daily life during the critical 45-69 window is what actually protects your heart.
Action Plan for Ages 45-69: What to Do Right Now
Stop reading and start doing. Here’s your plan.
This Week: Call your doctor and schedule a physical. Ask for a high-sensitivity troponin test, complete lipid panel, HbA1c test, and blood pressure check.
Go to the American Heart Association website and use their heart age calculator—it takes 5 minutes. Write down your Life’s Essential 8 scores so you know where you stand.
Next 3 Months: Walk 30 minutes, five days a week. No excuses. Plan your meals every Sunday—focus on vegetables, fish, whole grains, and olive oil. Go to bed at the same time every night. Make your room dark and cool. If you smoke, call 1-800-QUIT-NOW today. It’s free.
Long-Term: Check your numbers once a year. Take your medication if your doctor prescribes it. Find one person who’ll check in on your progress. Track your heart age every six months to see if it’s getting younger.
Call 911 Right Now If You Have: Chest pain, trouble breathing, irregular heartbeat, or dizziness. Don’t wait. Don’t “see if it gets better.”
These actions become even more powerful when you understand the latest advances in prevention and treatment available in 2025.
Your Heart’s Critical Window Starts Now

Your 40s, 50s, and 60s determine everything that follows. Silent heart damage now means dementia risk later—38% higher for people with elevated troponin. But here’s the good news: 17% of dementia cases are preventable by protecting your heart in middle age.
Life’s Essential 8 gives you the roadmap. Every factor is something you control.
This isn’t another article to bookmark and forget. If you’re between 45 and 69, this is your biological window. Call your doctor this week. Ask about high-sensitivity troponin testing. Calculate your heart age. Pick one metric from Life’s Essential 8 and improve it this month.
Your 80-year-old self—both your heart and your brain—will thank you.
Understanding when heart health decline accelerates fastest isn’t about fear—it’s about empowerment. The research is clear: middle age is your moment to act.






