A Top Cardiologist Reveals the 5 Things He Does Every Single Day for His Heart

Cardiovascular diseases (CVDs) remain the undisputed leading cause of death globally, responsible for an estimated 19.8 million lives lost in 2022 alone. In the United States, the statistics are just as staggering: nearly 128 million adults, or 48.6% of the population, are living with some form of cardiovascular disease. As a cardiologist, I see the downstream effects of this epidemic every day in my clinic.
But here is the single most important fact I share with my patients, and one that shapes my own life: The World Heart Federation maintains that at least 80% of premature deaths from heart attacks and strokes are preventable.
The problem isn’t a lack of information; it’s a lack of clarity. We are inundated with conflicting advice, fad diets, and “bio-hacks.” This article cuts through that noise. You’ve asked what I personally do every day to protect my own heart.

These five habits are not based on trends; they are my daily routine, built on the most current 2025 clinical guidelines and the foundational principles of preventative cardiology. This is the heart health actionable advice 2025 needs.
Habit 1: I Follow a Plant-Forward, Not Just Plant-Based, Diet
My first and most important habit is the food I eat. Diet is the foundational pillar of preventative cardiology and is the leading behavioral risk factor for preventable death in the U.S..

However, my approach is “plant-forward,” not necessarily strict plant-based. This distinction is crucial. My goal is a dietary pattern that emphasizes plants, best exemplified by the Mediterranean-style diet.
I follow the simple USDA MyPlate model: I fill half my plate with fruits and vegetables, one-quarter with fiber-rich whole grains, and one-quarter with a healthy protein. This automatically makes 75% of my plate plant-based.
This pattern is consistently associated with superior cardiovascular outcomes. A 2024 meta-analysis, for example, found that women with the highest adherence to a Mediterranean diet had a 24% lower risk of incident CVD and a 23% lower risk of total mortality.
I Strategically Swap My Fats
I don’t fear fat; I prioritize it. My daily habit involves a strategic swap: replacing saturated fats (SFAs) with unsaturated fats.
- Saturated Fats (I limit these): Found in red meats (beef, pork), full-fat dairy, and tropical oils like coconut and palm oil.
- Unsaturated Fats (I prioritize these): Found in foods like extra-virgin olive oil (the cornerstone of the MedDiet) , avocados, nuts, and seeds.
The data on this is unequivocal. A meta-analysis of high-quality trials, cited in an American Heart Association (AHA) Scientific Statement, showed that replacing SFA with unsaturated fats reduced cardiovascular disease risk by approximately 30%.
I Actively Eat Omega-3s (Fish) Twice a Week

This is a non-negotiable part of my weekly routine. The AHA recommends eating fish, particularly fatty fish, at least twice a week. I do this because their omega-3 fatty acids are powerful anti-inflammatories. Clinically, they are proven to lower triglycerides and may also help modestly lower blood pressure.
I Treat Red Meat as a “Special Occasion,” Not a Staple

This is a key 2025-era insight that goes beyond just saturated fat. When I replace a serving of red meat with a serving of fatty fish like salmon , I am executing a powerful “two-for-one” strategy for my heart:
- I remove: A source of saturated fat.
- I add: A potent anti-inflammatory (Omega-3s).
But there’s a third, less-known benefit. New research shows that when our gut microbes digest red meat, they produce a metabolite called TMAO (trimethylamine N-oxide).
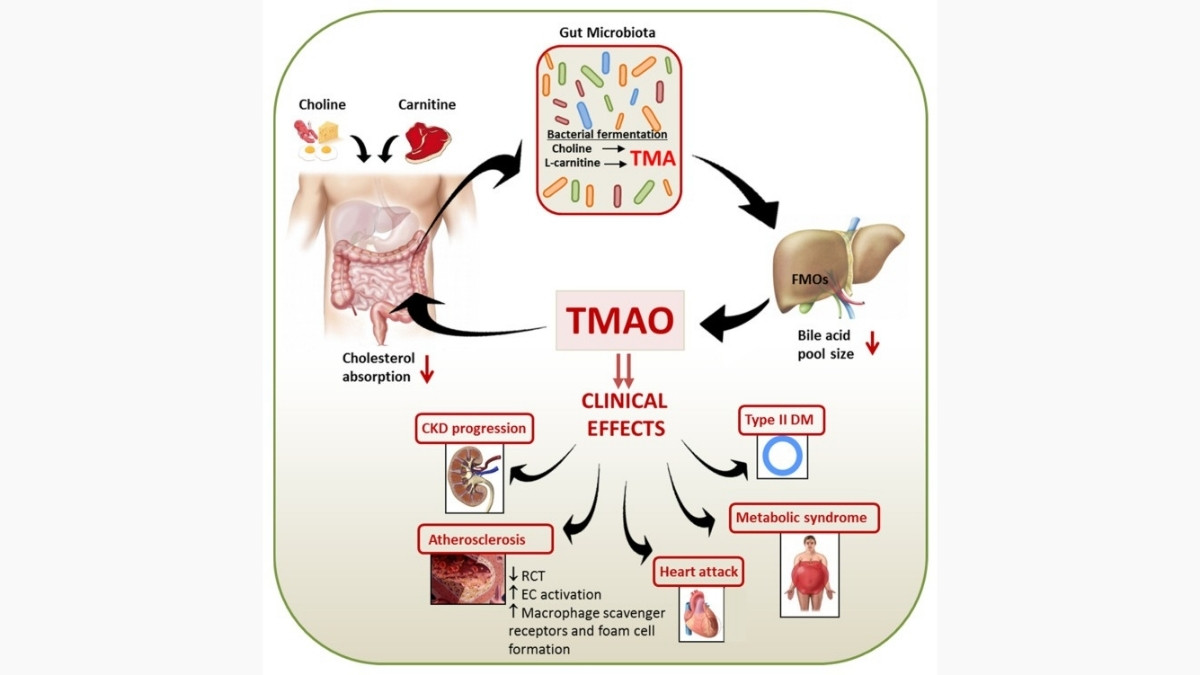
High blood levels of TMAO are directly associated with a higher risk for atherosclerotic cardiovascular disease (ASCVD), chronic kidney disease, and Type 2 diabetes. By limiting red meat, I am also limiting my TMAO production.
Your Actionable Step Today: Don’t overhaul your entire diet. Make one swap. This week, replace one red meat meal with a serving of fatty fish like salmon, mackerel, or sardines.
Habit 2: I Pair 150 Minutes of Cardio with Resistance Training

You already know the 2025 AHA guideline: get at least 150 minutes of moderate-intensity aerobic activity (like brisk walking or cycling) or 75 minutes of vigorous activity (like running) per week. This is my non-negotiable baseline.
But the “insider” habit, the one many people miss, is that I never skip resistance training. The 2025 guidelines are clear that aerobic and strength training are not interchangeable; they have different, complementary benefits for your heart.
The Strength “Booster”

My second habit is to add muscle-strengthening activity at least two days per week, as the AHA recommends. I do this for my blood lipids and metabolism. A 2024 AHA Scientific Statement confirmed that resistance training (using weights, bands, or bodyweight exercises like push-ups) has powerful cardiovascular benefits. It is proven to:
- Lower resting blood pressure.
- Decrease LDL (“bad”) cholesterol and triglycerides.
- Increase HDL (“good”) cholesterol.
In fact, the 2024 AHA statement noted that adults who participate in resistance training have approximately a 17% lower risk of CVD and a 15% lower risk of all-cause mortality.

For those short on time, research from Iowa State University (ISU) found that you can replace half of your aerobic workout with strength training to get the same cardiovascular benefits, plus the unique health benefits of improving your muscles.
Your Actionable Step Today: I follow a weekly template to ensure I get both. You can use it as a model.
Table 1: A Cardiologist’s Weekly Exercise Template (Meets 2025 AHA Guidelines)
📅 Your Complete Weekly Exercise Plan
A scientifically-balanced approach to cardiovascular health & strength
👇 Click each day to see detailed workout information!
- Vascular Health Improvement
- Blood Pressure Management
- Cardiovascular Endurance
- Lipid Management (LDL/HDL)
- Muscle Strength Building
- Metabolic Rate Enhancement
- Vascular Health Improvement
- Blood Pressure Management
- Aerobic Capacity Building
- Lipid Management (LDL/HDL)
- Muscle Strength Building
- Bone Density Improvement
- Vascular Health Improvement
- Blood Pressure Management
- Active Recovery
- Endurance Building
- Maximum Calorie Burn
- Cardiovascular Challenge
- Muscle Recovery
- Flexibility Maintenance
- Mental Relaxation
Habit 3: I Treat Sleep as a Non-Negotiable Prescription

In my clinic, I see the long-term effects of the “I’ll sleep when I’m dead” mindset. As cardiologist Dr. Dmitry Yaranov warns, this habit leads to “higher blood pressure, weight gain, and burnout you can’t shake”. Dr. Sudhir Kumar stated it perfectly: sleep is a “non-negotiable foundation for cardiovascular and metabolic recovery”.
The “U-Shaped” Risk Curve (Duration)

My sleep prescription is based on a well-established “U-shaped” risk curve: both too little and too much sleep are associated with greater mortality risk. The optimal duration for adults is 7-9 hours per night.
The risk of short sleep (<7 hours) is severe:
- High Blood Pressure: A 2024 American College of Cardiology (ACC) study found sleeping less than 7 hours was associated with a 7% increased risk of high BP. This risk spiked to 11% for those sleeping less than 5 hours.
- Cardiovascular Disease: A 2022 study found adults sleeping less than 6 hours had nearly triple the risk of developing cardiovascular issues.
- Atherosclerosis: Other studies show adults with 5 hours of sleep or less have a 200% to 300% higher risk of coronary artery buildup (plaque).
This happens because sleep deprivation fuels inflammation and raises stress hormones like cortisol , which are directly implicated in atherosclerosis.
The “Insider” Habit: Consistency

This is the true expert habit that I practice daily. When I sleep is as important as how long I sleep. New research (published in Hypertension) shows that people with irregular sleep patterns—meaning varying bedtimes and wake-times—have substantially higher odds of high blood pressure, even if they get the recommended 7-9 hours.
The latest 2025 research drives this point home. A study on heart failure patients found that having even moderately irregular sleep doubled the risk of re-hospitalization or death within six months.
My heart’s systems, especially blood pressure, are on a circadian rhythm. Sleep is when my blood pressure is supposed to “dip” and my body repairs. An irregular schedule disrupts this, keeping my body in a constant semi-stressed state.
Your Actionable Step Today:
I protect my sleep schedule with a strict hygiene routine. You can, too:
- Set a strict schedule: Go to bed and wake up at the same time every day, including weekends.
- Create a 1-hour “buffer”: No screens, or use a blue light filter. No heavy meals or alcohol within a few hours of bed.
- Optimize the environment: Keep your bedroom cool, dark, and quiet.
Habit 4: I Actively Manage Stress (I Don’t Just “Avoid” It)

As a cardiologist, I urge my patients (and myself) not to “brush off stress”. Chronic stress is not just a mental state; it is a physical, physiological state that directly drives heart disease.
The Cortisol-to-Heart-Disease Pathway
When I am chronically stressed, my body’s “fight or flight” alarm system is constantly on. This has two specific, negative consequences for my heart:
- Adrenaline: This hormone is released, causing my heart to beat faster and my blood pressure to rise.
- Cortisol: Prolonged release of this primary stress hormone increases my blood sugar, my “bad” LDL cholesterol, and my triglycerides.
This combination—high blood pressure, high lipids, and the systemic inflammation it causes —is the perfect recipe for damaging artery walls and creating plaque (atherosclerosis). In acute cases, severe stress can even lead to “Broken Heart Syndrome” (Takotsubo cardiomyopathy), a temporary heart failure state.
Furthermore, stress causes indirect damage by triggering poor health behaviors, such as overeating, smoking, poor sleep, and not taking medications as prescribed.
My “Active” Stress-Reduction Tools

My habit isn’t avoiding stress—that’s impossible. My habit is actively defusing it with intentional, daily parasympathetic (“rest and digest”) activation.
- Action 1: 5-Minute Mindfulness: I dedicate 5-10 minutes every day to practice a relaxation technique, such as deep breathing or meditation. Studies show these mindfulness practices can lower blood pressure and improve heart rate variability.
- Action 2: I Use Technology (Wisely): I use a meditation app. Apps like Headspace and Calm are excellent, evidence-based tools. Headspace is particularly good for beginners and has 3-minute “SOS meditations” to manage acute stress in the moment.
- Action 3: I Engage in a “Flow” Hobby: I schedule time for hobbies I enjoy, like playing music or gardening. Engaging in an enjoyable activity you love is a proven way to reduce cortisol, lower blood pressure, and slow your heart rate.
Your Actionable Step Today: Download the Headspace or Calm app. Before you even subscribe, try a free 5-minute guided breathing exercise.
Habit 5: I Know My “Big 4” Numbers (And My 2025 Targets)
This is the most important “doctor” habit of all. I cannot manage what I do not measure. This habit is the very foundation of preventative cardiology. I don’t guess about my health; I track my data. These are the “Big 4” numbers I know, based on the latest 2025 clinical guidelines.
1. Blood Pressure

This is the “silent killer.” I use a validated at-home blood pressure cuff. The 2025 AHA/ACC guidelines are the gold standard for these targets.
- Normal: Less than 120/80 mmHg
- Elevated: 120–129 systolic AND less than 80 diastolic
- Stage 1 Hypertension: 130–139 systolic OR 80–89 diastolic
2. Cholesterol (The Lipid Panel)

- LDL (“Bad”) Cholesterol: Lower is better.
- Optimal (Healthy Adults): Less than 100 mg/dL.
- Target (High-Risk/Post-Heart Attack): Less than 70 mg/dL.
- HDL (“Good”) Cholesterol: Higher is better.
- Optimal (Protective): Greater than or equal to 60 mg/dL.
- At-Risk: <40 mg/dL (men) or <50 mg/dL (women).
- Total Cholesterol: Optimal is less than 200 mg/dL.
3. Fasting Blood Glucose

This tracks my risk for prediabetes and Type 2 diabetes, which are major drivers of cardiovascular disease. The 2025 American Diabetes Association (ADA) Standards of Care set these levels:
- Normal: Less than 100 mg/dL
- Prediabetes: 100 mg/dL to 125 mg/dL
- Diabetes: 126 mg/dL or higher
4. Weight/BMI
I track my weight to ensure my Body Mass Index (BMI) stays in a healthy range, as obesity is a major risk factor.
Your Actionable Step Today: I’ve consolidated these targets into a single “scorecard.” Print this, and take it to your next doctor’s appointment.
Table 2: Your 2025 Cardiovascular Health Scorecard
🩺 Your Essential Health Metrics Guide
Know Your Numbers, Protect Your Health
👇 Click each metric card to see detailed ranges and action steps!
Using Technology as a Tool (With a Warning)
I use modern technology to track my habits and my biometrics. My Fitbit or Apple Watch tracks my daily steps, exercise minutes, and sleep consistency. For patients with palpitations, an FDA-cleared at-home ECG monitor like KardiaMobile is a fantastic tool for detecting arrhythmias like Atrial Fibrillation (AFib).
But this comes with a crucial “Doctor’s Warning,” which I borrow from cardiologist Dr. Daniel Fischman: “Don’t get overwhelmed or try to self-diagnose. There’s no such thing as ‘Dr. Watch'”. These devices are tools to inform a conversation with your physician, not a replacement for one.
A Cardiologist’s Conclusion,
These five habits are my daily defense system for my heart. They are not extreme, but they are consistent.
My diet and exercise (Habits 1 and 2) are the inputs that build a strong foundation. My sleep and stress management (Habits 3 and 4) are the regulators that keep the entire system running smoothly. And my numbers (Habit 5) are the data that proves the system is working.
You do not need to master all five habits by tomorrow. The journey to preventative heart health starts with a single step. Pick one. This week, schedule your 30-minute walks or buy that at-home blood pressure cuff.
Start today. These cardiologist daily habits for heart are the foundation of preventative cardiology and can give you the heart health actionable advice you need for 2025 and beyond.






