Which Calcium Supplement Actually Builds Bone vs. Calcifies Arteries? Research Reveals The Shocking Truth

A 2024 study tracked nearly 400 patients for five years. The results should scare anyone taking calcium pills. Those who took calcium supplements had more calcium building up in their arteries. But their bones? No stronger than before.
Right now, millions of people swallow calcium supplements every day. They think they’re protecting their bones from breaking.
But new research shows many are doing the opposite—depositing calcium in their arteries instead of their skeleton. This is called the calcium paradox, and it’s left people confused and scared.
Here’s the good news. You can fix this today.
In this article, you’ll learn why calcium supplements affect your arteries differently than calcium from food. You’ll discover the critical nutrients that tell calcium where to go in your body—your bones, not your blood vessels.
I’ll show you which forms of calcium actually build bone versus which ones calcify arteries. You’ll get the exact supplement protocol backed by 2024-2025 research. And you’ll learn how to get calcium from food sources that don’t carry any heart risk.
Your calcium supplement might be hurting you. Let’s fix that right now.
The Calcium Paradox: What Recent Research Reveals
Here’s something that should scare you: A 22-year study of women taking calcium and vitamin D supplements found they had a 6% higher chance of dying from heart disease. Not lower. Higher.

This seems crazy. We take calcium to get stronger bones, right? But here’s what’s actually happening in your body.
When you swallow a calcium pill, all that calcium hits your bloodstream at once. It’s like dumping a bucket of water on a plant instead of watering it slowly. Your body can’t handle the flood.
A Canadian study proved this. Women who took calcium supplements had more calcium building up in their arteries. But women who ate the same amount of calcium from food? Their arteries stayed clean.
The worst part? After five years, the supplement users had more artery problems AND their bones weren’t any stronger. They got the risk without the benefit.
Scientists call this the “bolus effect.” That’s a fancy way of saying too much, too fast. Your body tries to put the calcium in your bones. But when there’s too much calcium floating around, it ends up in your artery walls instead. Like putting mail in the wrong mailbox.
Food releases calcium slowly. Your body can handle that. Supplements dump it all at once. That’s the difference between building bone and clogging arteries.
The Missing Link: Why Vitamin K2 Changes Everything
There’s a vitamin that tells calcium where to go in your body. Most people have never heard of it. It’s called vitamin K2.

Think of K2 as a traffic cop for calcium. Without it, calcium wanders around lost. It ends up in your arteries instead of your bones.
K2 does two important jobs. First, it turns on a protein called MGP that stops calcium from sticking to your artery walls. Second, it activates another protein called osteocalcin that grabs calcium from your blood and stuffs it into your bones where it belongs.
A study in Denmark proved this works. People taking statins also took 720 micrograms of K2 with vitamin D every day. Their artery calcification slowed way down.
Another study looked at kidney disease patients. They took just 90 micrograms of K2 (the MK-7 type) with vitamin D. Their arteries got thicker much slower than people who only took vitamin D.
The biggest proof? The Rotterdam study tracked 4,809 people for years. Those who ate more K2 in their diet had fewer heart attacks and lived longer. Their arteries stayed cleaner too.
Here’s the dose that works: 75 to 120 micrograms daily. Look for MK-7 on the label. It stays in your body longer than other types.
Calcium Citrate vs. Carbonate: The Absorption Difference
Citrate vs. Carbonate
Pick the right one or waste your money
Citrate
ABSORPTION RATE- Taking acid-reducers (Nexium/Prilosec)
- Age 60+ (Low acid)
- Sensitive stomach / IBS
Carbonate
CALCIUM CONTENT- Normal stomach acid
- Budget-conscious (Cheaper)
- No acid-blocker meds
Your body absorbs these two types completely differently. Pick the wrong one and you’re wasting money.
Calcium citrate gets absorbed 22% to 27% better than carbonate. That’s a big deal. One study found citrate was actually 2.5 times more bioavailable. Your body uses more of what you swallow.
Here’s the catch. Carbonate has more actual calcium per pill—40% versus 21% in citrate. So you need to take more citrate pills to get the same amount. But if your body can’t absorb carbonate well, those extra milligrams don’t help you anyway.

Carbonate needs stomach acid to work. Take it with food or it just passes through. Citrate works either way—empty stomach or with meals.
Choose citrate if you:
- Take Prilosec, Nexium, Pepcid, or other acid-reducing drugs
- Are over 60 (stomach acid drops with age)
- Have digestive problems or IBS
Choose carbonate if you:
- Have normal stomach acid
- Want to save money (it’s cheaper)
- Don’t take acid-blocking medications
One more rule for both types: Never take more than 500 mg at once. Your body can only absorb so much calcium at a time. Split bigger doses into morning and night.
Food First: The Safest Calcium Sources
CALCIUM: The Safe Way
The Calcium Paradox: Countries with highest milk consumption have highest fracture rates.
South Africa (196mg/day) = 9x fewer fractures than USA.
NOON: Sardine Salad (325mg)
PM: Tofu Stir-fry + Bok Choy (540mg)
Food gives you calcium the safe way. It enters your blood slowly, so your body can handle it properly. No artery problems.
Here’s something weird: Countries that drink the most milk have the highest rates of broken bones. South Africans get only 196mg of calcium daily but have nine times fewer hip fractures than Americans. More calcium doesn’t always mean stronger bones.
But absorption matters more than the amount you eat. One cup of bok choy gives you 70% absorption—you actually use 132mg out of the 190mg in there. Milk only absorbs at 32%, so you get 96mg from the 300mg in a cup.
Best calcium foods you can eat today:
Dairy lovers: Plain yogurt (400mg per cup), milk (300mg), cheese (200mg per ounce)
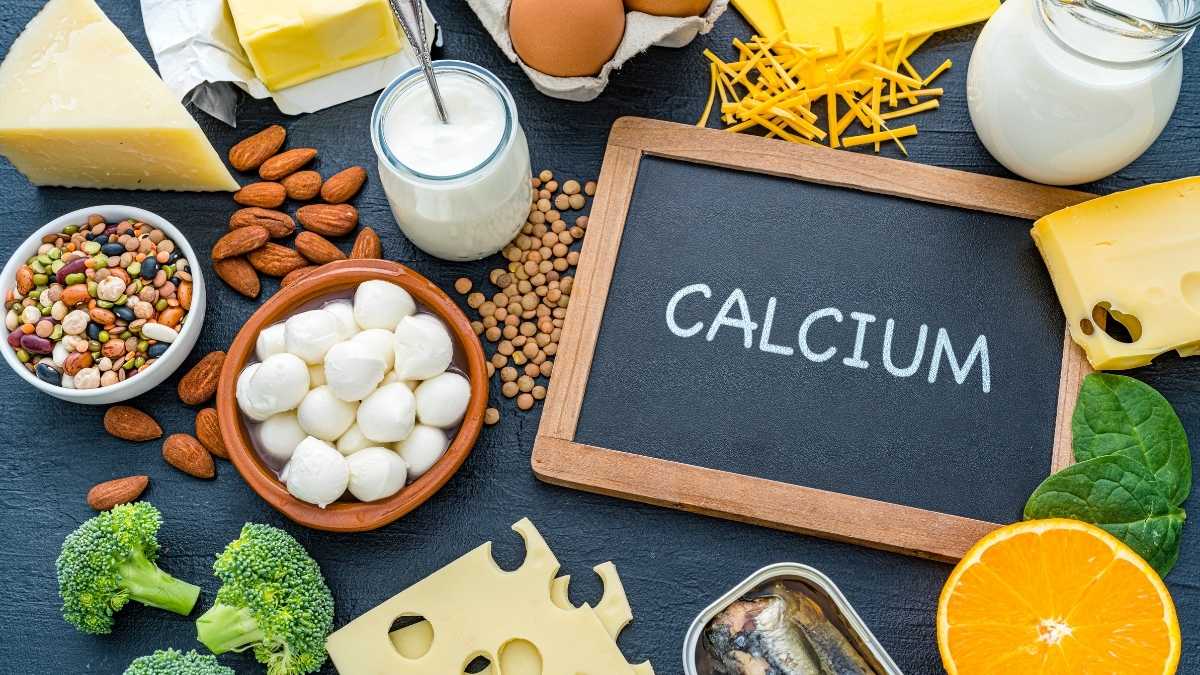
No dairy? Try these: Sardines with bones (325mg per 3oz can), firm tofu (350mg per half cup), bok choy (190mg per cooked cup)
Sneaky sources: Sesame seeds (88mg per tablespoon—sprinkle on everything), chia seeds (76mg per tablespoon), dried figs (121mg per half cup)
Fortified options: Soy milk (300mg per cup), fortified orange juice (300mg per cup), fortified cereal
Easy 1,000mg day: Breakfast: Fortified orange juice (300mg) + chia seed pudding (76mg) Lunch: Sardine salad (325mg) Dinner: Tofu stir-fry with bok choy (540mg)

The Evidence-Based Supplement Protocol (2025 Update)
Most people don’t need calcium pills if they eat right. Track your food for three days first. If you’re getting 1,000mg daily from food, skip the supplements.
You DO need supplements if you’re a woman past menopause, over 70 years old, can’t digest dairy, or eat a restricted diet. Otherwise, stick with food.
The complete stack that actually works:
Never take calcium alone. Here’s what research says you need together: Calcium citrate 500mg (twice daily), Vitamin K2 as MK-7 form (90-180 mcg daily), Vitamin D3 (1,000-2,000 IU daily), Magnesium citrate or glycinate (200-400mg daily)
Timing matters more than you think:
Your body can only absorb 500mg of calcium at once. More than that just gets wasted. Take K2 and D3 with a meal that has fat—peanut butter, eggs, cheese. They won’t work without fat.

Keep calcium away from your other pills. It blocks iron, zinc, and thyroid medication. Wait 2-4 hours between them.
What to look for on the label:
Third-party tested stamps (USP, NSF, or ConsumerLab). K2 listed as “MK-7” specifically. Magnesium as citrate, glycinate, or malate—NOT oxide. Zero bone meal, dolomite, or oyster shell (they contain lead).
Your daily schedule:

Morning with breakfast: 500mg calcium citrate + 90 mcg K2-MK7 + 1,000 IU D3
Evening with dinner: 500mg calcium citrate + 200mg magnesium glycinate
Never go over 2,000mg total calcium per day from all sources
Testing Your Calcium Status: Beyond Basic Supplements
You can’t fix what you don’t measure. Here are the tests that show if calcium is helping or hurting you.
CAC Score (Coronary Artery Calcium): This CT scan shows how much calcium is stuck in your heart arteries. It’s the best test for artery health. Get one if you’re over 40 or have heart disease risk factors like high blood pressure or diabetes. A score of zero is perfect. Above 100 means you need to act fast.
DEXA Scan: This measures bone density. Women need one at 65, men at 70. Get it earlier if you’ve broken bones easily, take steroids, or have a family history of osteoporosis. The test takes 10 minutes and doesn’t hurt.

Blood Tests You Need:
Vitamin D (25-OH test): Check yearly. You want 30-50 ng/mL. Below 20 means you’re deficient and can’t absorb calcium right.
Serum calcium: Makes sure you’re not getting too much.
Parathyroid hormone (PTH): High levels mean your body is stealing calcium from your bones.

Uncarboxylated osteocalcin: Shows if you need more K2. Not all labs offer this yet, but ask anyway.
Test first. Supplement second. That’s how you know what’s actually working.
The Bottom Line: Get Calcium Right
You now know why some calcium builds bone while other calcium clogs arteries. It’s not the calcium itself—it’s how you take it.
Three things make the difference. First, the form matters. Citrate absorbs better than carbonate. Second, you need helpers. K2 and magnesium aren’t optional—they tell calcium where to go. Third, food beats pills every time. Your body handles food calcium safely.
The 2024-2025 research is clear. Taking calcium alone is old advice that can hurt you. Don’t do it.

Here’s what to do today:
Track your food calcium for three days. Add up what you’re actually eating. Most people get more than they think.
If you need supplements, buy the right ones. Calcium citrate with K2-MK7 and magnesium together. Not calcium alone.
Get tested. A CAC score shows your artery health. A DEXA scan shows your bone health. You need both numbers.
Start with food. Sardines, yogurt, bok choy, tofu, fortified orange juice. Real food gives you calcium plus all the other nutrients that make it work.
Your bones deserve calcium that actually reaches them—not supplements that end up calcifying your arteries instead. Now you know how to make that happen.