The 15 Early Warning Signs of Dementia I Had at 59—I Addressed Them All and My Cognition at 66 Is Perfect

When I couldn’t remember my grandson’s name at his birthday party, I knew something was terribly wrong—but what happened next changed everything.
At 59, I stood in my kitchen staring at the coffee maker I’d used for 10 years. I couldn’t remember how to turn it on. That moment sent me to doctors, through cognitive tests, and into a complete lifestyle overhaul.
Maybe you’re forgetting conversations. Maybe you’re worried these memory problems mean dementia. Maybe you feel helpless about your brain health and don’t know what’s normal aging versus serious cognitive decline.
Seven years later, my cognitive function tests show improvements that surprised even my neurologist. I’ll show you the 15 early warning signs I experienced, the difference between mild cognitive impairment and dementia, and the seven science-backed interventions that worked.
This is my story—and the dementia risk factors you can actually change starting today
The 15 Early Warning Signs I Experienced (And Why I Almost Ignored Them)

I thought I was just stressed. Everyone forgets things, right? But when my wife pointed out I’d asked her the same question three times in an hour, I couldn’t brush it off anymore.
The memory problems got worse.
I’d finish a phone call with my sister and have no memory of what we discussed. At my grandson’s soccer game, I forgot which kid was mine. I missed a dentist appointment I’d written down three times.
Then came the word problems. Mid-sentence, simple words would vanish. I’d say “that round thing” instead of “clock.” My colleagues noticed me trailing off, losing my point halfway through meetings.
Basic tasks became confusing. Paying bills online—something I’d done for years—suddenly felt like solving a puzzle. Making breakfast took twice as long. I’d stand in the grocery store, forgetting why I came.
Driving scared me. I got lost going to my daughter’s house. I misjudged a turn and scraped my bumper. Reading the newspaper required extra focus because words seemed to blend together.
My mood changed too. Social events made me anxious. I snapped at my wife over nothing. A dark cloud of depression settled in, something I’d never experienced before.
These weren’t isolated incidents—they were patterns. Around 45% of dementia cases could be prevented by addressing 14 modifiable risk factors, The Lancet according to the 2024 Lancet Commission report. Recognizing these early signs of dementia gave me my best chance at intervention.
What My Neurologist Found: MCI vs. Dementia (And Why It Matters)
Dr. Martinez ran me through a series of tests. The MoCA test asked me to draw clocks, remember words, and solve simple problems. I scored 24 out of 30. Normal is 26 or higher.
The MRI showed my brain structure looked okay. No tumors, no strokes. Blood tests ruled out thyroid problems and vitamin deficiencies. The genetic test revealed I carry one copy of the APOE ε4 gene, which increases risk but doesn’t guarantee anything.
But here’s what changed everything. “You have Mild Cognitive Impairment,” Dr. Martinez said. “Not dementia.”
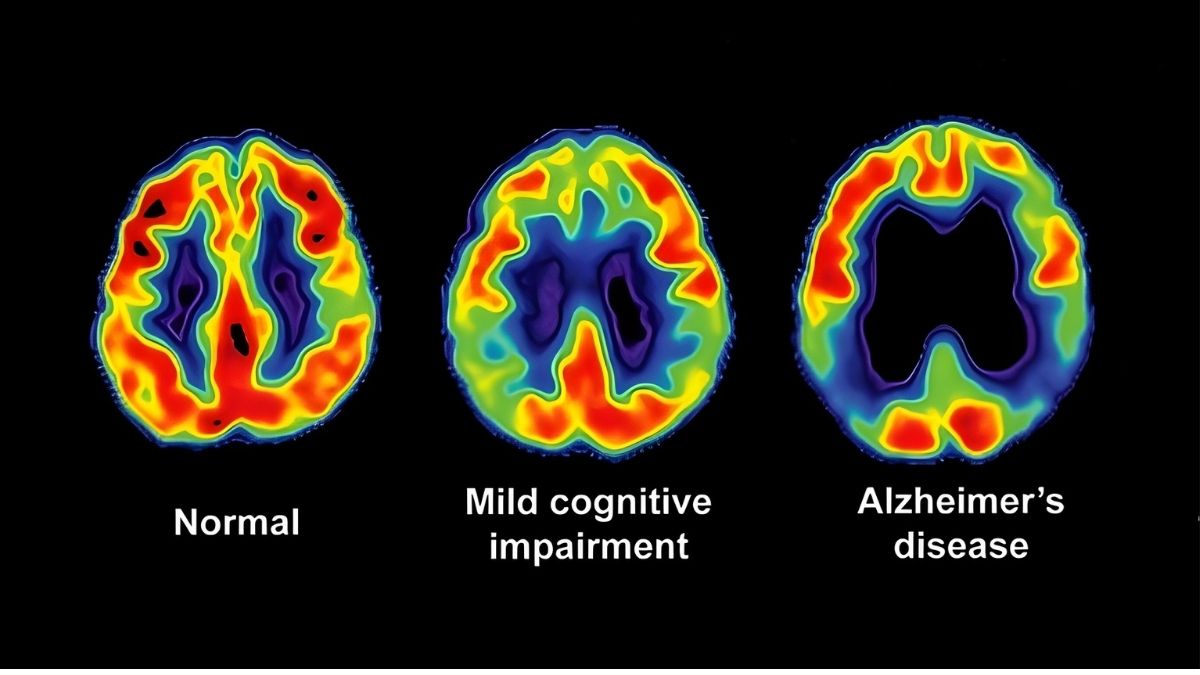
MCI means your thinking problems are worse than normal aging but not bad enough to be dementia. You can still handle daily life. Between 10-20% of people over 65 have MCI. Some get worse. Some stay the same. And here’s the crucial part—some actually improve.
The neurologist explained something crucial. Dementia means you can’t function independently anymore. MCI means you still can. That gap is your window to act.
Research shows hearing aids alone reduced cognitive decline by 48% over three years Alzdiscovery. Your brain can still change and adapt. Scientists call this brain plasticity. The earlier you catch problems, the more you can do about them.
This distinction would prove critical to everything that came next.
The 14 Modifiable Risk Factors: What 2024 Research Reveals
The 2024 Lancet Commission dropped a bombshell. Nearly 45% of dementia cases could be prevented by fixing 14 specific problems. Not maybe. Not theoretically. Actually prevented.
I had seven of these dementia risk factors. Seven chances to change my future.
Early Life (What’s Done Is Done) Less education increases risk by 5%. I couldn’t change my high school diploma at 59, so I moved on.
Midlife Factors (Ages 45-65) Hearing loss accounts for 7% of risk. I got hearing aids within a month. Hypertension adds 9%—my blood pressure was 145/92. Obesity contributes 3%—I was 35 pounds overweight. Depression adds 3%—I’d been feeling down for months. I had a concussion at 40 from a car accident, adding 2% risk.
Late Life Factors (65+) Physical inactivity causes 6% of cases. I was barely moving. Social isolation adds 4%—I’d stopped seeing friends. Diabetes increases risk by 2%—my A1C was creeping up. Vision loss, new in 2024, adds 2%—I needed stronger glasses but kept putting it off. High LDL cholesterol, also new for 2024, contributes 1%—mine was 190.
Smoking (5%) and excessive alcohol (1%) weren’t my problems. Air pollution (2%) was hard to control where I lived.
Here’s what matters. Just cutting salt intake could prevent over 43,000 dementia cases. These brain health modifiable factors weren’t genetic destiny. They were choices I could make starting that day.
I targeted six factors I could actually fix.
The 7 Interventions That Changed My Brain Health
I left Dr. Martinez’s office with a choice. Accept decline or fight back with science. I chose to fight.
Intervention 1: The MIND Diet Revolution

The MIND diet combines Mediterranean and DASH eating plans. It targets foods that protect your brain. Research shows people who follow it closely cut Alzheimer’s risk by 53%. Even moderate followers see 35% risk reduction.
I cleaned out my kitchen in one weekend. Out went the butter, cheese, and red meat. In came blueberries by the flat, spinach by the bag, and walnuts by the pound. The changes were dramatic but necessary.
Here’s what I ate on a typical day. Breakfast was oatmeal with blueberries and walnuts. Lunch featured a massive spinach salad with grilled salmon, olive oil, and chickpeas. Dinner included brown rice, roasted vegetables, and baked chicken or fish. Snacks were almonds or an apple.
The shopping list got simple. Leafy greens six times weekly. Berries every other day. Nuts daily. Fish twice weekly. Beans three times weekly. Whole grains three servings daily. Olive oil for everything.
What I cut way back: Red meat to once monthly. Butter and margarine almost gone. Cheese became rare. Pastries and sweets for special occasions only.
The difference in brain function was equivalent to being 7.5 years younger according to studies. Within three months, my afternoon brain fog lifted. My cholesterol dropped 40 points without medication.
Start small if this feels overwhelming. Week one, add berries to breakfast. Week two, swap one meat meal for fish. Week three, use olive oil instead of butter. Week four, eat a big salad for lunch daily.
I tracked my meals using a simple notebook. No fancy apps needed. Just accountability.
Intervention 2: Exercise Protocol

Just 35 minutes of moderate activity per week cuts dementia risk by 41%. That’s five minutes daily. I started there and built up.
Week one looked pitiful. Twenty-minute walks twice weekly. I was winded and sore. But I kept going.
Six months later, here’s my schedule. Monday: 30-minute brisk walk plus 20 minutes strength training. Tuesday: Swimming for 40 minutes. Wednesday: Rest or gentle yoga. Thursday: HIIT workout (20 minutes of intense intervals). Friday: 45-minute walk. Saturday: Resistance bands and bodyweight exercises. Sunday: Longer walk or hike.
The science backs this up. Midlife exercise lowers dementia risk by 41%. Starting in late life still gives 45% reduction. Vigorous exercise works best—126 minutes weekly shows major benefits. But even 5,000-7,500 steps daily helps significantly.
I mixed it up to stay interested. Walking, swimming, lifting weights, yoga for balance. Variety kept me engaged and worked different systems.
Your starting point: Pick one activity you don’t hate. Walk for 20 minutes twice this week. Next week, add five minutes. The month after, add a third day. Build slowly. Your brain benefits even from small amounts.
I bought a cheap fitness tracker. Seeing my steps climb from 2,000 to 8,000 daily kept me motivated.
Intervention 3: Cognitive Training

Your brain needs exercise too. Three 30-minute sessions weekly improves memory and thinking. Crossword puzzles may delay decline by 2.5 years. Number puzzles daily can make your brain perform like it’s eight years younger.
I made brain training part of my routine. Every morning with coffee, I did the crossword puzzle. Lunch break meant 15 minutes on a brain training app. Evenings, I practiced Spanish on Duolingo.
What actually worked: Daily crosswords challenged my vocabulary and memory. Learning Spanish forced my brain to create new pathways. Chess games with my grandson combined social time with strategy practice. Reading challenging books instead of watching TV.
Free tools I used: Library newspapers for puzzles. Duolingo for language learning. YouTube chess tutorials. The library itself for harder books.
Paid option that helped: I tried Lumosity for three months. It was okay but not magic. The free stuff worked just as well with more discipline.
The key was variety and challenge. When crosswords got easy, I switched to cryptic puzzles. When basic Spanish felt comfortable, I joined a conversation group.
You can start today. Download Duolingo. Pick up a puzzle book at the dollar store. Learn something that scares you a little.
Intervention 4: Cardiovascular Health Optimization

My blood pressure was 145/92. My LDL cholesterol hit 190. My A1C crept toward prediabetes. Every number screamed danger for my brain.
Here’s what changed. I monitored blood pressure at home twice weekly. Numbers on a chart made it real. The MIND diet and exercise dropped my pressure to 125/80 in four months without medication.
My doctor prescribed a statin for cholesterol. Combined with diet changes, my LDL fell to 110. My A1C went from 5.9 to 5.4, pulling me back from diabetes.
The monitoring routine: Blood pressure every Sunday and Wednesday morning. Doctor visits every three months initially, now every six months. Home A1C test kit quarterly. Weight daily.
Research shows controlling these factors protects your brain directly. Blood vessels in your brain need the same care as vessels in your heart. High blood pressure damages them. High cholesterol clogs them. High blood sugar harms them.
Your action steps: Buy a blood pressure cuff (under $30). Check your numbers. Share them with your doctor. Ask about targets. Follow up monthly until you hit goals.
Intervention 5: Hearing Correction

I’d been saying “what?” constantly for three years. Hearing loss accounts for 7% of dementia risk. The ACHIEVE trial showed hearing aids cut cognitive decline by 48% over three years.
I got tested immediately. Moderate hearing loss in both ears. Hearing aids cost me $2,400 but insurance covered half. Within weeks, I noticed the difference.
What improved beyond hearing: I stopped avoiding social situations. Conversations didn’t exhaust me anymore. My wife stopped repeating everything. I felt less isolated and confused.
If you’re asking people to repeat themselves, get tested. Many insurance plans now cover hearing aids. Some cost as little as $200 per ear.
Intervention 6: Social Engagement

Social isolation adds 4% to dementia risk. I’d stopped seeing friends. I’d quit my book club. I was alone too much.
I forced myself back out. Rejoined the book club. Volunteered at the food bank Tuesday mornings. Started a weekly coffee meetup with old colleagues. Called my sister every Sunday.
The resistance was real. My anxiety made me want to cancel every time. But showing up consistently got easier. Social connection protects your brain while fighting depression and isolation simultaneously.
Start small: Text one friend this week to meet for coffee. Say yes to the next invitation you get. Find one group that meets your interests.
Intervention 7: Sleep and Stress Management

Poor sleep and chronic stress were killing my brain. Depression made everything worse.
My sleep hygiene overhaul: No screens after 9 PM. Bedroom kept cool and dark. Same bedtime every night (10:30 PM). No caffeine after 2 PM. Reading instead of TV before bed.
I learned basic meditation using a free app. Ten minutes daily. It felt silly at first but helped my stress levels drop noticeably.
My doctor briefly prescribed an antidepressant. Combined with exercise and social connection, my depression lifted after six months. I tapered off medication under supervision.
The compound effect: Better sleep improved my energy for exercise. Lower stress helped my blood pressure. Treating depression made social engagement easier. Everything connected.
These seven interventions became my daily practice. Not easy—but nothing important ever is.
My Cognitive Function at 66: What the Tests Show

Seven years after that terrifying morning in my kitchen, I sat across from Dr. Martinez again. This time, the test results told a different story.
The numbers improved. My MoCA score went from 24 to 28. Normal range. My processing speed tests showed marked improvement. Memory recall that had been in the 40th percentile now hit the 75th percentile for my age group.
Dr. Martinez was cautiously optimistic. “This is exactly what we hope to see with aggressive lifestyle intervention,” she said. The US POINTER study backs this up—structured lifestyle changes improved cognitive function equivalent to being 1-2 years younger.
Daily life changed dramatically. I remember conversations now. I don’t repeat questions. I manage my finances without confusion. My grandson’s name comes instantly. The coffee maker is just a coffee maker again, not a puzzle.
My wife noticed first. “You’re back,” she said one morning. My kids stopped exchanging worried glances when I spoke.
But I’m not cured. Some things still take longer than they used to. I write more lists than before. Under stress, word-finding gets harder. This isn’t a miracle—it’s management.
I still do everything I started seven years ago. The MIND diet. The exercise. The brain training. Stop any of it, and I slide backward.
These cognitive improvement results required work. They still do.
Your Personalized Action Plan: Where to Start Today
You don’t need to do everything I did on day one. Start small. Build momentum. Here’s your roadmap for how to prevent dementia starting right now.
Step 1: Get Evaluated This Week

Call your doctor Monday morning. Say you’re concerned about memory changes and want cognitive testing. Request a MoCA or MMSE test. Ask for complete blood work including vitamin B12, thyroid function, and A1C. Get your blood pressure and cholesterol checked.
Questions to ask: “Could anything else be causing these symptoms?” “What’s my baseline cognitive score?” “Which risk factors apply to me?” “What specialists should I see?”
Write down the answers. Bring someone with you if possible. Anxiety makes it hard to remember everything.
Get baseline measurements now. Weight, blood pressure, cholesterol, blood sugar, cognitive test scores. You can’t track progress without a starting point.
Step 2: Identify Your Risk Factors Today

Go through the 14 factors honestly. Check which ones apply to you. Less education? Can’t change it. Hearing loss? Fixable. High blood pressure? Fixable. Smoking? Fixable. Physical inactivity? Fixable.
Rank them by ease. Some changes are simple. Adding a daily walk costs nothing. Getting hearing aids takes money and time. Quitting smoking is hard but critical. Focus on what you can do this month.
Find your low-hanging fruit. If you’re inactive, movement is your first target. If you eat fast food daily, diet is priority one. If you’re isolated, social connection comes first.
Step 3: Start Small This Week

Pick ONE intervention. Just one. Maybe it’s walking 20 minutes three times this week. Maybe it’s adding berries and spinach to your meals. Maybe it’s doing a crossword puzzle daily.
Set a stupidly easy goal. So easy you can’t fail. Walk for 10 minutes if 20 feels impossible. Eat one serving of leafy greens if six seems crazy. Do one puzzle if daily feels overwhelming.
Track it simply. Use your phone’s notes app. Mark an X on a calendar. Tell someone your goal and report back. Tracking creates accountability.
Build gradually over months. Week one: 10-minute walks. Week five: 15-minute walks. Week nine: 20-minute walks plus one strength session. Slow progress beats no progress every time.
Step 4: Build Your Team

You can’t do this alone. Tell your family what you’re doing and why. Ask for support. “I need you to walk with me twice weekly.” “Please don’t bring cookies home.” “Remind me if I forget my hearing aids.”
Find an accountability partner. A friend making similar changes. A spouse. A sibling. Someone who checks in weekly and celebrates small wins with you.
Join a group. Walking clubs. Online support forums. The Alzheimer’s Association offers free programs. Community centers have exercise classes. Connection plus activity equals double benefit.
Lean on professionals. Your doctor. A dietitian. A personal trainer. A therapist if depression is part of your picture. Insurance often covers these.
Step 5: Create Systems That Stick

Meal planning Sunday afternoons. Write your menu for the week. Shop once. Prep what you can. Remove decision fatigue from weeknight dinners.
Exercise scheduling like appointments. Put it in your calendar. Monday 7 AM walk. Wednesday 6 PM yoga. Saturday morning swim. Treat it like a doctor’s appointment you can’t miss.
Brain training with your coffee. Link new habits to existing ones. Coffee means crossword puzzle. Lunch break means Duolingo. Bedtime means reading instead of TV.
Monitoring routine monthly. First Sunday of every month, check blood pressure, weight, and cognitive activities log. Every three months, doctor appointment. Every six months, cognitive testing.
First week actions: Call doctor. Start tracking one habit. Add berries to breakfast or take one 15-minute walk.
First month goals: Complete medical evaluation. Establish one new habit consistently. Research hearing test or other needed specialist.
Three-month milestones: Two interventions running consistently. Baseline measurements repeated. Initial improvements visible in energy or mood.
One-year vision: Multiple interventions as natural routine. Measurable cognitive improvements. Risk factors reduced. Quality of life better.
At the Last,
At 59, standing in my kitchen unable to work my coffee maker, I thought my life was over. Those early warning signs felt like a death sentence. They weren’t. They were a wake-up call.

Here’s what I know now. Nearly 45% of dementia cases can be prevented. The science is clear. The interventions work. Starting matters more than perfecting.
You have more control than you think. Fourteen modifiable risk factors means fourteen chances to change your trajectory. Some require money. Some require time. All require commitment. But dementia prevention starts today with one small decision.
The tools exist right now. The MIND diet costs no more than junk food. Walking is free. Crossword puzzles cost a dollar. Hearing tests are covered by Medicare. Brain training apps have free versions. You don’t need expensive programs or magic pills.
Don’t wait for a crisis. If you’re experiencing any warning signs I described, talk to your doctor this week. If you have risk factors, address them now. Your future self will thank you.
Start with one change. Take a 20-minute walk twice this week. Add leafy greens to your lunch. Call about that hearing test you’ve been avoiding. Download Duolingo. Do today’s crossword puzzle.
Small actions, sustained over time, create remarkable changes in your brain health. I’m living proof. My cognitive decline can be slowed, managed, and in some measures reversed. Yours can be too.
At 59, I was terrified. At 66, I’m empowered. The difference wasn’t luck—it was information, action, and commitment. Brain health is achievable. Your journey starts with the next decision you make.
Make that decision today.






