The Bedroom Habit That’s Secretly Straining Your Heart

It’s not the late-night phone scrolling or the midnight snack. The most dangerous bedroom habit straining your heart might be one you’re not even awake for.
You wake up feeling like you haven’t slept. Your energy crashes by 2 PM, and maybe your doctor has even mentioned your rising blood pressure. You blame stress or aging, but the real culprit could be hiding in plain sight every night.
This article uncovers that hidden habit: untreated sleep apnea. We will show you exactly how sleep apnea affects the heart. You’ll also learn why snoring and heart disease are linked and the simple signs you must stop ignoring.

😴 Sleep Apnea: The Hidden Epidemic
🔄 What Happens During Sleep Apnea
❤️ How Sleep Apnea Damages Your Heart
🚨 7 Key Warning Signs You Can’t Ignore
⚖️ Top 5 Risk Factors for Sleep Apnea
🎯 Your Treatment Journey
👥 Partner’s Guide: What to Watch For
✨ Life Before vs After CPAP Treatment
The “Secret” Revealed: What Is Obstructive Sleep Apnea?
The “secret” bedroom habit is obstructive sleep apnea, or OSA. It’s a condition where the muscles in your throat relax too much during sleep. This relaxation causes your airway to narrow or close completely.
This blockage means you actually stop breathing for 10, 20, or even 30 seconds at a time. Your brain senses the lack of oxygen and hits a panic button. It forces you to partially wake up—just enough to gasp, take a breath, and clear the airway.

Here’s the “secret” part: you almost never remember these micro-awakenings. This cycle can happen hundreds of times a night, completely wrecking your sleep quality. You just think you slept poorly, or your partner complains about loud, gasping snores.
This issue is more common than most people think. According to the American Medical Association, nearly 30 million Americans have OSA. Yet, a shocking 80% of moderate and severe cases remain undiagnosed, leaving people at risk.
How This Nightly Habit Is Straining Your Heart
When you stop breathing, your blood oxygen level plummets. Your brain thinks you are in danger and hits the “fight-or-flight” panic button. It floods your body with stress hormones like adrenaline.

This hormone surge makes your heart pound and tightens your blood vessels. This causes a sharp, sudden spike in your high blood pressure. This isn’t a one-time thing; it happens over and over, all night long.
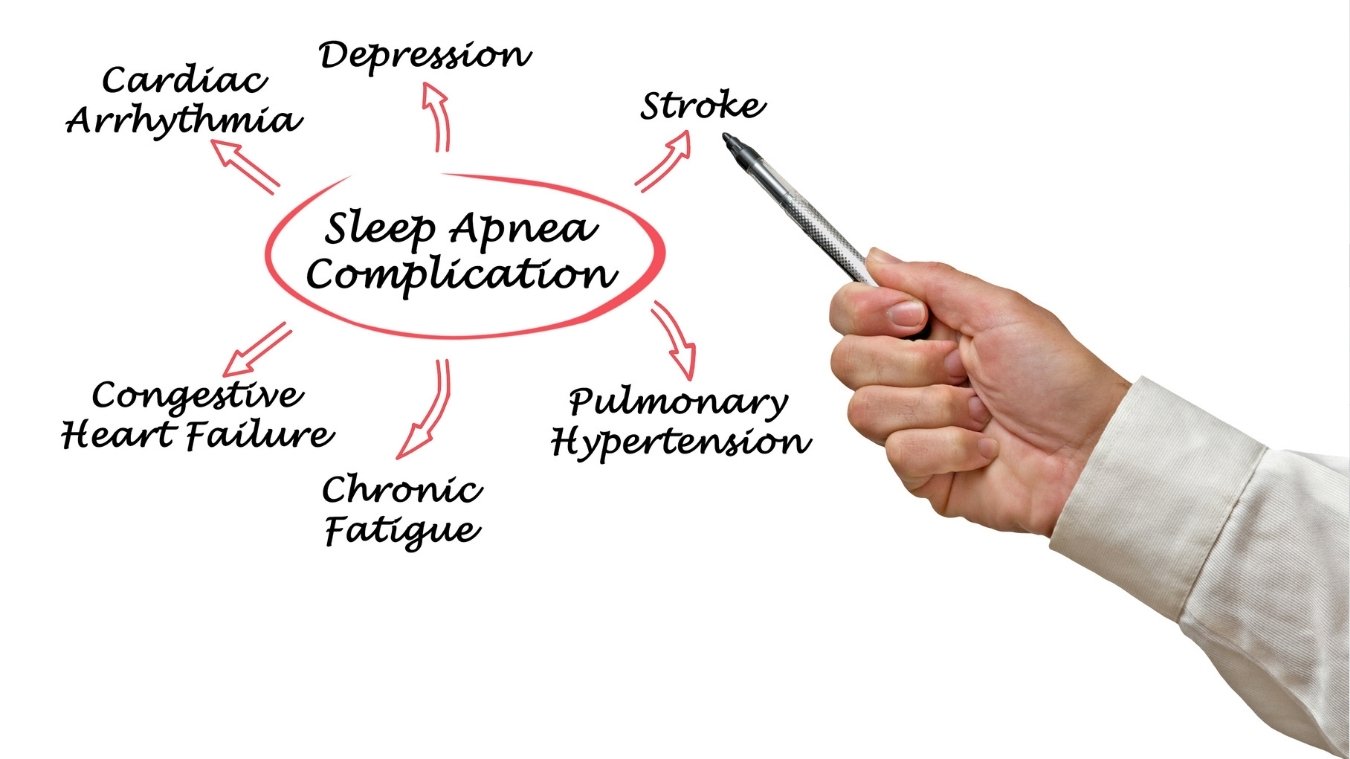
This nightly cycle is exactly how sleep apnea affects the heart. All that chronic stress is straining your heart while you sleep. This leads to serious damage, like chronic high blood pressure (hypertension) even during the day.

The strain can also trigger an irregular heartbeat called atrial fibrillation (A-fib). A study from the American Heart Association shows people with severe sleep apnea are two to four times more likely to get A-fib. Over time, this damage increases your risk of heart attack and stroke.
Are You at Risk? 7 Key Signs of Sleep Apnea
You might be ignoring the signs of sleep apnea because you’re asleep when they happen. Ask yourself, or your partner, if these warnings sound familiar.
- Loud, Persistent Snoring This isn’t a light rumble. It’s loud snoring that’s often interrupted by choking or gasping sounds.
- Observed Pauses in Breathing Your partner may notice that you stop breathing for several seconds at a time while you sleep.
- Excessive Daytime Fatigue This is the biggest red flag. It’s not just “being tired.” It’s a deep exhaustion that stays with you even after a full night’s sleep, making it hard to get through the day.
- Waking Up With Headaches Frequent morning headaches are a common sign, often caused by low oxygen levels during the night.
- Dry Mouth or Sore Throat You might wake up with a very dry mouth or sore throat from gasping for air.
- Difficulty Concentrating This “brain fog” can make it hard to focus, remember things, or stay productive at work.
- Stubborn High Blood Pressure If you have high blood pressure that is difficult to control, even with medication, sleep apnea could be a major reason.
How to Reclaim Your Sleep and Protect Your Heart
The good news is that sleep apnea is very treatable. Your first step is to talk to your doctor. Don’t self-diagnose; explain your symptoms and concerns about snoring and heart disease.
Your doctor will likely recommend a sleep study to get a clear diagnosis. This might be a simple at-home test you can do in your own bed, or a more detailed in-lab study. Both will show if you are stopping breathing.
The most effective sleep apnea treatment is often a CPAP machine. Think of it like a gentle, constant “air splint.” It sends a steady stream of air through a mask to keep your airway open so you can breathe easily all night.

For milder cases, other options might include special oral appliances or lifestyle changes like weight loss. The payoff is huge: treatment doesn’t just stop snoring. It can lower your blood pressure, reduce your risk for A-fib, and give you your energy back. This is how you protect your heart.
A Guide for Partners: What to Do If You Hear the “Silence”
If you are the partner, you are often the only one who knows the full story. You are the witness to the scariest part. Your help is essential because you see what they cannot.
Simple snoring is just a sound. The real danger is the silence between snores. That’s the “apnea,” when my partner stops breathing for 10 seconds or more. It often ends with a loud snort, a choke, or a partner snoring gasping for air.

How do you bring this up? Don’t say, “Your snoring is awful.” Instead, try: “I’m worried about you. I heard you stop breathing last night, and it scared me.” You can even try recording the sound on your phone. Hearing the gasp for themselves is often what they need.
Encourage them to see a doctor for sleep apnea help. The goal is to convince partner to get sleep study. A solution, like a CPAP machine, protects their heart. And, it means you will finally get a quiet, peaceful night of sleep, too.
Who Is Most at Risk? 5 Factors That Increase Your Chances
Some people are more likely to develop sleep apnea than others. Here are the five biggest sleep apnea risk factors that put you in the danger zone.
1. Excess Weight (The #1 Risk Factor)
Carrying extra weight is the single biggest cause of sleep apnea. Fat deposits around your upper airway physically squeeze your throat, making it collapse when you sleep. This is the direct link between weight and sleep apnea.

Even losing 10-15 pounds can significantly improve symptoms. If you’re overweight, this is the most powerful change you can make.
2. Physical Anatomy (It’s Not Just About Weight)
Your body structure matters too. A neck circumference greater than 17 inches for men and 16 inches for women is a strong predictor of increased risk for obstructive sleep apnea.

Other physical traits that increase risk:
- A narrow throat or small airway
- Large tonsils or adenoids
- A recessed chin or jaw (your lower jaw sits farther back)
- A thick tongue base
You can’t change these traits, but knowing them helps you watch for symptoms.
3. Age and Gender (Risk Changes Over Time)
Sleep apnea becomes more common as you age. Your throat muscles naturally weaken over time, making airway collapse easier.

Men are 2-3 times more likely to have sleep apnea than younger women. But here’s the catch: a woman’s risk increases dramatically after menopause. Hormonal changes reduce muscle tone in the throat, closing the gender gap.
4. Lifestyle Habits (What You Do Matters)
Three habits make sleep apnea worse by relaxing your throat muscles:
Alcohol: Drinking before bed relaxes throat muscles for hours, increasing airway collapse.

Sedatives and sleeping pills: These medications have the same effect as alcohol—they relax muscles that should stay firm.
Smoking: Irritates and inflames the upper airway, causing swelling that narrows your breathing passage. Smokers are three times more likely to have sleep apnea.
5. Family History (Genetics Play a Role)
If your parents or siblings have sleep apnea, your risk increases. Genetics influence your airway size, muscle tone, and how your body controls breathing during sleep.
You can’t change your genes, but you can control the other four factors. Focus on what you can fix.
Lastly:
That “harmless” snoring or constant exhaustion is more than just annoying. It can be a clear warning sign of sleep apnea. This is a bedroom habit that is secretly straining your heart every single night.
Ignoring these signs is a risk your heart can’t afford. If this sounds like you, or your partner, it’s time to talk to a doctor.
Getting this checked is a critical step. Taking your sleep seriously is one of the best things you can do for your sleep apnea and heart health.