I’m Living With Dementia at 60. Here’s What I Wish EVERYONE Knew (Especially My Family)
When I received my dementia diagnosis at 60, the world suddenly saw me differently. Friends stopped calling, colleagues whispered in hallways, and family members began speaking about me instead of to me.
Society assumes dementia only affects the elderly, leaving younger people like me invisible and misunderstood. The isolation hits harder than the memory loss, and misconceptions create barriers where support should exist.
What I’ve learned living with early-onset dementia could change how you interact with people like me. These insights come from daily experience, not medical textbooks.
Understanding the real challenges we face helps families communicate better, communities offer meaningful support, and society break down harmful stereotypes. Knowledge bridges the gap between fear and compassion, creating connections that benefit everyone involved.
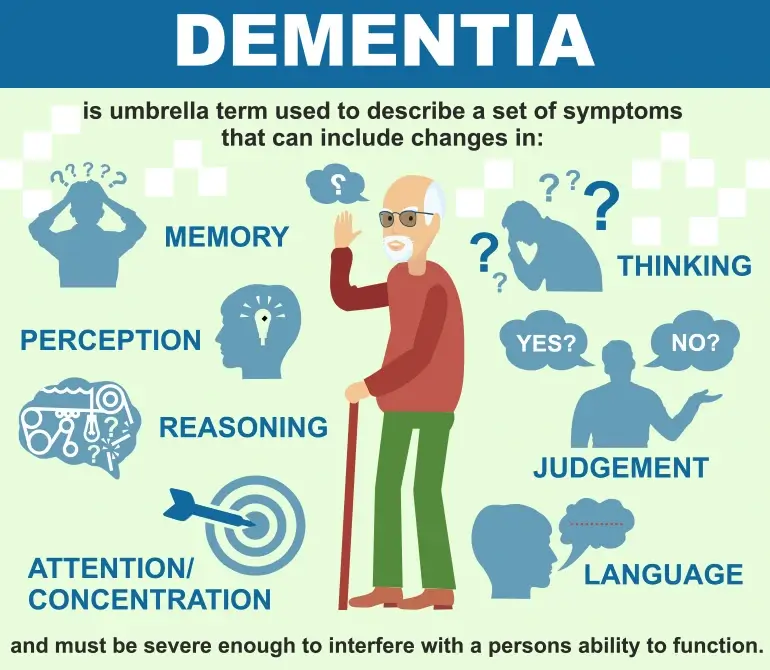
“Dementia”
Dementia is a general term for a decline in cognitive function severe enough to interfere with daily life, affecting memory, thinking, and behavior. It is caused by damage to brain cells, often due to diseases like Alzheimer’s. Symptoms worsen over time, and there is currently no cure, only treatments to manage symptoms.
More than 55 million people worldwide experience dementia, Dementia is the seventh leading cause of death globally, and Alzheimer’s disease is the most common form of dementia.1
The Diagnosis Shock: It’s Not Just an “Old Person’s Disease”
When the neurologist said “early-onset dementia,” I stared at him in disbelief. At 60, I was supposed to be planning retirement, not facing cognitive decline. Society paints dementia as something that happens to people in their 80s and 90s.

The reality hits differently when you’re still working, still driving, still living independently. About 200,000 Americans under 65 have early-onset dementia, yet most people don’t know we exist. My doctor explained that genetics, not age, was the primary factor in my case.
The stereotype of the confused elderly person in a nursing home doesn’t match my experience. I’m learning that dementia doesn’t wait for you to be “old enough.”
I’m Still Me Inside – My Personality Hasn’t Disappeared
My sense of humor remains intact, even when words escape me. People seem surprised when I make jokes or express opinions about current events. Yes, I forget names and lose track of conversations, but my core self hasn’t vanished.

I still love jazz music, get excited about baseball games, and worry about my grandchildren. My preferences haven’t changed; my ability to express them has. Friends sometimes speak to me like I’m a child, using simple words and slow speech.
This hurts more than they realize. I may stumble over complex thoughts, but I still have them. My personality shines through the fog of confusion. The essence of who I am remains strong.
1. The Workplace Nightmare: When Your Career Ends Overnight
Telling my boss about the diagnosis felt like signing my professional death certificate. Within weeks, I went from respected manager to liability risk. Colleagues started excluding me from important meetings, claiming they were “protecting” me from stress.
The HR department suggested early retirement before I was ready to leave. My 35-year career ended not with celebration, but with whispered conversations and awkward goodbyes. The Americans with Disabilities Act offers some protection, but workplace discrimination is subtle and hard to prove.
Financial planning becomes urgent when your earning years are cut short. I went from breadwinner to dependent in six months. The loss of professional identity stings as much as the lost income.
2. Stop Talking About Me Like I’m Not Here
Standing right beside someone while they discuss your condition with others is dehumanizing. Family members often ask my wife about my symptoms instead of asking me directly. I’m present in the room, aware of the conversation, yet treated like furniture.

Healthcare providers sometimes address my spouse exclusively, as if my diagnosis erased my voice. This behavior makes me feel invisible and strips away my dignity. I can still answer questions about my own experience, thank you very much.
My cognitive challenges don’t mean I’ve lost the right to participate in decisions about my life. Speaking directly to me shows respect for my remaining abilities. Include me in conversations about my own care and future.
3. My Memory is Broken, But My Emotions Are Amplified
Forgetting where I put my keys is frustrating, but the emotional impact hits like a tsunami. Small disappointments feel catastrophic; moments of joy become overwhelming. My brain’s emotional regulation system seems to be working overtime while my memory fails.

I cry more easily now, sometimes over things that wouldn’t have bothered me before. Anger flares up quickly, often surprising both me and my family. These aren’t personality changes; they’re symptoms of how dementia affects emotional processing.
My feelings are more intense, not less meaningful. Understanding this helps my family respond with patience instead of alarm. The emotions are real, even when the triggers seem small.
4. The Isolation is Real – When Friends Start Disappearing
Social invitations stopped coming after word spread about my diagnosis. Friends who once called regularly now avoid me, unsure how to act around someone with dementia. Some people fear the disease might be contagious, which sounds ridiculous but happens more often than you’d think.

Others simply don’t know what to say, so they say nothing at all. The silence hurts worse than awkward conversations ever could. My social circle shrunk from dozens to a handful of brave souls who stuck around. Loneliness becomes a daily companion when the world treats you like damaged goods.
Community support groups help, but they can’t replace lifelong friendships. Staying connected requires effort from both sides, yet most people choose the easier path of avoidance.
5. I Need Routine, Not Chaos – Why Structure Saves My Sanity
Unexpected changes send my brain into overdrive, creating confusion where none existed before. Simple routines like morning coffee at 8 AM and evening news at 6 PM anchor my day. When family members rearrange furniture or change meal times, my world tilts sideways.

Familiar environments help my brain navigate daily tasks without constant decision making. New places exhaust me because every detail requires conscious thought instead of automatic response. My bathroom supplies stay in the same spots; my keys hang on the same hook.
This isn’t stubbornness; it’s survival strategy. Predictable patterns free up mental energy for more important things. Small changes feel enormous when your cognitive resources are already stretched thin.
6. Don’t Correct Me Every Time – Sometimes It’s Better to Go Along
Constant corrections make every conversation feel like a test I’m failing. When I call my grandson by his brother’s name, pointing out the mistake doesn’t help anyone. My brain knows something is wrong; your corrections just add shame to confusion.

Sometimes joining my reality works better than forcing me into yours. If I think it’s Tuesday when it’s Wednesday, correcting me won’t improve my memory. Choose your battles wisely and save corrections for truly important matters.
Safety issues need addressing, but harmless mistakes can slide by. Your patience means more than your accuracy. Let me finish thoughts even when they take longer than usual.
7. My Independence Matters More Than Your Worry
Overprotective family members want to wrap me in bubble wrap, but I’m not ready for that life yet. Taking away my car keys before I’m unsafe steals more than transportation; it removes my freedom. Yes, I might get lost occasionally, but I also might surprise you with my resourcefulness.

Risk assessment should involve my input, not just your fears about what might happen. I understand the balance between safety and autonomy, but the decision should be mine while I’m still capable.
Helicopter parenting doesn’t work with adults, even adults with dementia. Trust me to know my own limits until I prove otherwise. Your worry comes from love, but it can suffocate the life I’m trying to live.
8. The Good Days and Bad Days – Stop Expecting Consistency
Yesterday I cooked a complete dinner; today I burned toast. This rollercoaster of ability confuses everyone, including me. Some mornings my mind feels sharp and clear; other days feel like walking through thick fog. Family members get frustrated when I can remember song lyrics from 1970 but forget what I had for breakfast.
Brain function doesn’t follow a predictable pattern with dementia. Good days give false hope; bad days bring despair. Neither represents my true baseline because there isn’t one anymore.
Planning activities becomes challenging when you can’t predict your cognitive state. Accept the fluctuations instead of fighting them. Celebrate clear moments without expecting them to last forever.
9. Technology Can Be My Best Friend or Worst Enemy
Simple apps on my phone help me remember appointments and medication times. Voice assistants answer questions when words escape me, becoming my external memory bank. However, software updates turn familiar interfaces into confusing puzzles overnight.

My tablet reminds me to call my daughter, but the same device frustrates me when new features appear without warning. Smart home devices can announce the weather and play my favorite music with voice commands. Complex passwords and security questions become impossible hurdles when memory fails.
Large button phones work better than smartphones with tiny icons and multiple functions. Technology should adapt to my changing needs, not force me to relearn everything constantly. Choose tools that solve problems instead of creating new ones.
10. I’m Not Giving Up – I’m Adapting and Finding New Ways to Live
Crossword puzzles got too hard, so I switched to jigsaw puzzles that engage my brain differently. Reading novels became challenging, but audiobooks let me enjoy stories again. My garden keeps me active even when indoor tasks feel overwhelming.

Exercise routines adapted to my abilities help maintain physical health while boosting mood. Art classes provide creative outlets that don’t require perfect memory or complex thinking. Volunteering at the animal shelter gives me purpose and social interaction without pressure.
Each day brings small victories worth celebrating, like remembering a friend’s name or completing a simple task. Hope lives in adaptation, not in fighting against inevitable changes. Life continues; it just looks different than I planned.
11. My Caregiver Needs Care Too – This Affects the Whole Family
Watching my wife struggle with exhaustion breaks my heart more than my own confusion. She carries the weight of both our futures while pretending everything is fine. Caregiver support groups help her process emotions she can’t share with me. Our adult children feel guilty living their own lives while Mom handles everything alone.

Family dynamics shift when one person becomes the primary caregiver without preparation or training. Respite care gives her breaks, but she feels guilty leaving me with strangers.
Financial strain hits everyone when one income disappears and medical costs increase. Professional counseling helps family members cope with grief for the person I used to be. Everyone needs support, not just the person with dementia.
12. Legal and Financial Planning: The Conversations We Must Have Now
Power of attorney documents got signed while I could still understand their implications. Advance directives spell out my wishes for medical care when I can’t speak for myself. Financial accounts need accessible organization before confusion makes banking impossible.

Insurance policies require review to understand what coverage exists for long term care. Estate planning becomes urgent when cognitive decline threatens decision making ability. Family members need to know where important documents are stored and how to access them.
These conversations hurt because they acknowledge a future where I can’t manage my own affairs. Waiting too long means losing the legal capacity to make these critical decisions. Planning now protects everyone later, even though it feels like giving up control.
What I Want My Legacy to Be – Beyond This Disease
Stories about my life before dementia matter more than tales of my decline. Grandchildren should remember my bad jokes and weekend fishing trips, not just my confused moments. Photo albums capture happy memories that will outlast my ability to recall them.

Family recipes I taught my daughter preserve traditions that connect generations. The vegetable garden I planted will feed the family long after I forget how to tend it. Letters I’m writing now will speak for me when words no longer come easily.
Community volunteer work created friendships and positive impact that extends beyond my diagnosis. This disease is just one chapter in a much longer story of love, work, and relationships. Remember me as I lived, not just how I’m leaving.
Lastly,
Living with dementia at 60 has taught me that dignity doesn’t disappear with memory loss. Each day brings challenges, but also moments of connection and joy that remind me why life remains worth living. My family has learned to see beyond the diagnosis to the person who still laughs, loves, and contributes to their world.
This journey isn’t about surrendering to disease; it’s about adapting with grace while maintaining hope. Communities need to understand that dementia affects real people with ongoing dreams and relationships.
Support comes in many forms, from simple conversation to respite care for overwhelmed caregivers. Most importantly, early-onset dementia doesn’t define me or limit my capacity to teach others about resilience. The conversation starts here, but it doesn’t end with my story.